Direct oral anticoagulants were associated with decreased bleeding risk versus warfarin in a recent retrospective analysis of primary care databases.
Apixaban (Eliquis) was associated with decreased risk of major bleeding events versus warfarin both in patients with atrial fibrillation (AF) and those prescribed anticoagulants for other causes, according to study results.
Rivaroxaban (Xarelto) was associated with a decrease in risk of intracranial bleeding, compared with warfarin in patients without AF, as was dabigatran (Pradaxa), reported Yana Vinogradova, a research statistician in the division of primary care at the University of Nottingham, England, and her coauthors.
An increased risk of all-cause mortality was seen with both rivaroxaban and low-dose apixaban, possibly because more patients died of age-related causes while on these direct oral anticoagulants (DOACs), they reported.
“This large observational study, based on a general population in a primary care setting, provides reassurance about the safety of DOACs as an alternative to warfarin across all new incident users,” Ms. Vinogradova and her colleagues said in the BMJ.
Evidence establishing the noninferiority of DOACs to warfarin comes mostly from controlled trials in AF leaving “residual concerns” about the safety of these newer agents in real world settings, where a broader range of patients may receive them, they added.
Accordingly, they conducted an analysis based on patient data from two U.K. primary care databases that were representative of the national population, according to the researchers.
A total of 196,061 patients were represented in the study, including 103,270 (53%) with AF and 92,791 (47%) who received anticoagulants for other reasons.
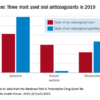
A total of 67% of patients received warfarin, though its use declined from 98% in 2011, the beginning of the study period, to 23% in 2016, the end of the study period. Over that same time period, use of rivaroxaban rose from 1% to 42%, and use of apixaban rose from 0% to 31%, while dabigatran use peaked in 2013 at 10%, dropping to 3% by 2016.
Edoxaban was excluded from the study because it was not licensed in the United Kingdom until the end of 2015, investigators said.
For patients with AF, apixaban was linked to a lower major bleeding risk, both versus warfarin (adjusted hazard ratio, 0.66; 95% confidence interval, 0.54-0.79) and versus rivaroxaban, the published data show. Apixaban was associated with a lower risk of intracranial bleed versus warfarin in patients with AF (aHR, 0.40; 95% CI, 0.25-0.64) as was dabigatran (aHR, 0.45; 95% CI, 0.26-0.77).
For patients without AF, apixaban was again associated with a lower risk of major bleeding versus warfarin and versus rivaroxaban, while rivaroxaban was associated with lower intracranial bleeding risk versus warfarin, and apixaban with lower risks for gastrointestinal bleeds.
Compared with apixaban, rivaroxaban and dabigatran were associated with higher risks of certain bleeding events, further analyses show.
Rivaroxaban and lower-dose apixaban were both associated with increased all-cause mortality risk versus warfarin, both in the atrial fibrillation and non-AF groups, Ms. Vinogradova and her coinvestigators noted.
“A greater proportion of the older patients on apixaban and rivaroxaban may have died while still taking anticoagulants but from age-related causes other than ischemic stroke or venous thromboembolism,” they wrote.
Compared with patients on higher doses of DOACs, patients receiving lower doses were older and had more comorbidities and more previous events, they added.
Between DOACs, results of this particular analysis were most favorable for apixaban, according to investigators.
“Our study has shown that the risk of major bleeding is lower in patients taking apixaban regardless of the reason for prescribing,” they wrote. “This was most pronounced for intracranial bleeding in patients with atrial fibrillation and for gastrointestinal bleeding in patients without atrial fibrillation, appearing, in general, to show apixaban to be the safest drug.”
© Frontline Medical Communications 2018-2021. Reprinted with permission, all rights reserved.