It’s the stuff of doctors’ nightmares. In a recent analysis of attitudes, beliefs, and practices regarding opioid prescribing, one hospitalist described how a patient had overdosed: “She crushed up the oxycodone we were giving her in the hospital and shot it up through her central line and died.”1
Another hospitalist recounted how a patient, after having her gallbladder removed, asked for a prescription to tide her over until she could see her primary care physician. “I later found out she had forged my script and had changed it from 18 pills to 180 pills. She took it all over the state to try to fill.”
Susan Calcaterra, MD, MPH, of the department of family medicine at the University of Colorado at Denver, Aurora; a hospitalist at Denver Health Hospital; and lead author of the recent study, says that the dramatic anecdotes don’t surprise her. “These are not uncommon events,” she said. “Across the country, you hear about overdose, you hear about people abusing fentanyl, and I think, when you have an addiction, your judgment of the dangers associated with your personal opioid use may be limited.”
Some critics have blamed the ubiquity of opioid prescriptions on the controversial movement to establish pain as a vital sign. Multiple investigations also have accused the pharmaceutical industry of aggressively promoting these prescription drugs while downplaying their risks. The CDC found that, in fact, so many opioid prescriptions were being written by 2012 that the 259 million scripts could have supplied every U.S. adult with his and her own bottle. In August 2017, President Trump declared the opioid crisis a national emergency, although opinions differ regarding the best ways forward.
Until recently, however, few studies had looked at how inpatient prescribing may be fueling a surging epidemic that already has exacted a staggering toll. So far, the early data paint a disturbing picture that suggests hospitals are both a part of the problem and a key to its solution.
“This has been a very, very rapidly evolving change from very little opioid use to widespread opioid use with the belief that there weren’t consequences,” said Hilary Mosher, MD, FHM, of the department of internal medicine at the University of Iowa in Iowa City. Hospitalists have to own their role in contributing to the current reality, she said, while also recognizing their power and responsibility to be agents of change. “We’re learning as we’re going,” said Dr. Mosher, who is also a hospitalist with the Iowa City Veterans Affairs Health Care System. “I think rather than looking back and saying, ‘Oh, my gosh, what have we done? Look at everything we did wrong,’ we’ve got to assess where we are and say, ‘How do we do right?’ ”
Illuminating a ‘black box’
Changing the trajectory will be difficult. From 2002 to 2015, the nation’s overdose death rate from opioid analgesics, heroin, and synthetic opioids, such as fentanyl, nearly tripled, and studies suggest that prescription painkillers have become major gateway drugs for heroin.2 In the last 3 years alone, fentanyl-related deaths soared by more than 500%, and annual mortality from all drug overdoses has blown by the peak of the HIV/AIDS epidemic in 1995, when nearly 51,000 died from the disease.3
Amid the ringing alarm bells, hospitals have remained a largely neglected “regulatory dead zone” for opioids, said Shoshana Herzig, MD, MPH, of the department of medicine at Harvard Medical School, Boston, and director of hospital medicine research at Beth Israel Deaconess Medical Center, also in Boston. In an editorial accompanying the recent study of hospitalist perspectives, Dr. Herzig called the inpatient setting an opioid prescribing “black box.”4
In a previous analysis of 1.1 million nonsurgical hospital admissions, however, she and colleagues found that opioids were prescribed to 51% of all patients.5 More than half of those with inpatient exposure were still taking opioids on their discharge day. With other studies suggesting that such practices may be contributing to chronic opioid use long after hospitalization, Dr. Herzig wrote, “reigning in inpatient prescribing may be a crucial step in curbing the opioid epidemic as a whole.”
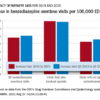
A recent study led by Anupam Jena, MD, PhD, a health care policy expert at Harvard Medical School, echoes the refrain. “It’s kind of remarkable that the hospital setting hasn’t really been studied, and it’s an important setting,” he said. When he and colleagues did their own analysis of hospitalized Medicare beneficiaries, they found that 15% of previously opioid-naive patients were discharged with a prescription.6 Of those patients, more than 40% remained on opioids three months after discharge. The research also revealed a nearly two-fold variation in prescription rates across hospitals.
Study coauthor Pinar Karaca-Mandic, PhD, a health economist at the University of Minnesota School of Public Health in Minneapolis, said the group’s research was motivated by a prior study in which they found that more than 30% of Medicare beneficiaries with opioid prescriptions were getting them from multiple providers.7 Nearly two-thirds of those prescriptions were concurrent. Although the study couldn’t assess appropriateness, Dr. Karaca-Mandic said that concurrent prescriptions from multiple providers correlated with higher rates of opioid-related hospitalization.
Some hospitalists have asserted that the increase in opioid prescriptions may partially be tied to pressure to reduce 30-day readmission rates; Dr. Jena and Dr. Karaca-Mandic’s work leaves open the possibility that such prescriptions may increase readmissions instead. The researchers, however, say a bigger driving force may be financial pressure tied to discharging patients earlier or scoring higher on quality measures that gauge factors, such as pain management. Hospitals that scored better on HCAHPS measures of inpatient pain control, their study found, were slightly more likely to discharge patients on opioids.
Keri Holmes-Maybank, MD, MSCR, FHM, an academic hospitalist at the Medical University of South Carolina, Charleston, says a lack of clear evidence and guidelines, unrealistic expectations, and variable patient responses to opioids are compounding a “very frustrating and very scary” situation for hospital medicine. Hospitalists who conclude that a patient-requested antibiotic will do more harm than good, for example, usually feel comfortable saying no. “But a patient can talk you into an opioid,” she said. “It’s much harder to stand your ground with that, even though we need to be viewing it the same way.”