In April 2015, President Obama signed the bipartisan Medicare Access and CHIP Reauthorization Act (MACRA) into law, effectively altering the future of the Medicare payment system for providers. MACRA not only removed the Sustainable Growth Rate, but also encouraged quality measure development, expanded the use of Medicare data, and locked provider payment rates to near zero growth.
For Medicare payments, MACRA created the Quality Payment Program, which breaks down clinical payments into two pathways: the Merit-Based Incentive Payment System (MIPS) combining current pay-for-performance programs into one consolidated payment system, and Alternative Payment Models (APMs), incentivizing payment models that move away from a fee-for-service system.
Starting in 2019, clinician Medicare payment adjustments will depend on which track the provider or the provider’s hospitalist group chooses to participate in. The Centers for Medicare & Medicaid Services will use 2017 data to determine 2019 payment adjustments.
Both pathways incur risk, as well as rewards:
• MIPS. –4% penalty up to 12% positive adjustment in year 1 based on 2017 data reported and collected by the CMS, growing over time to include payment adjustments from –9% to +27% in future years.
• APMs. If the provider is eligible, a 5% payment increase from 2019 to 2024, with no reporting requirements, and exemption from MIPS.
Who is included in the program?
All clinicians who receive Medicare Physician Fee Schedule payments, including physicians, physician assistants, and nurse practitioners, will be affected by this program. The only providers who are exempt from the program are those who fall under low-volume thresholds (either less than $30,000 in Medicare Part B charges or less than 101 Medicare patients) or those in their first year with Medicare.
The majority of hospitalists will fall into the MIPS pathway, at least for 2017.
What is MIPS?
MIPS requires reporting in four categories that determine a physician’s payment adjustment:
• Quality, which replaces the Physician Quality Reporting System (PQRS).
• Cost, which replaces the value-based modifier.
• Advancing Care Information (ACI), which replaces the meaningful use program.
• Improvement activities, a new category, but one in which hospitalists should excel, as they are already participating in many of the activities.
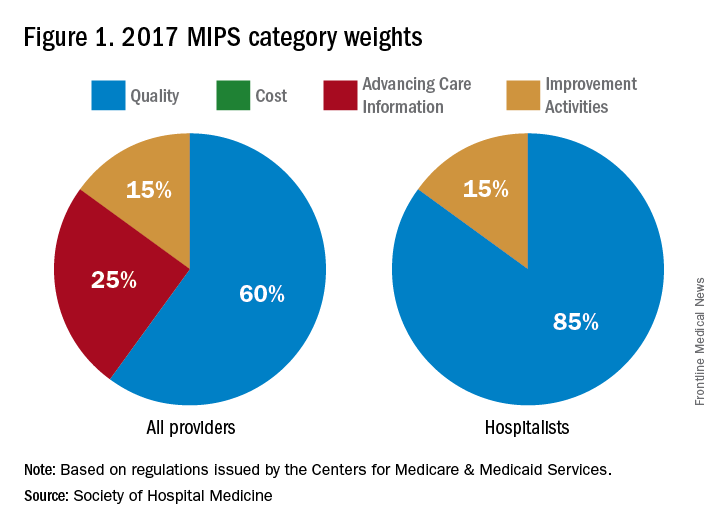
Each category is given relative weight, which the CMS will adjust in the first few years of the program.
Note that in the first year (2017), cost will be calculated, but not used to determine payment amount, hence this category gets a 0% weighting. Also, there are significant differences between how most providers’ MIPS score will be calculated with respect to category weights, and how this will be done for hospitalists.
In addition to cost, the ACI will not play a role in the 2019 performance scores for hospitalists. However, hospitalists who practice in noninpatient settings, such as skilled nursing facilities or ambulatory clinics, will be subject to the ACI unless they apply for exceptions.
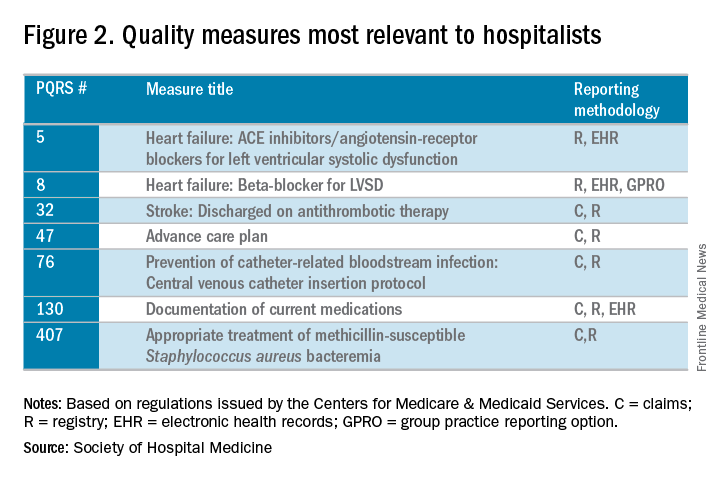
The quality category requires physicians to report on 6 of the 271 measures available. Hospitalists can report from the hospitalist-specific specialty set for which the Society of Hospital Medicine (SHM) was successful in advocating. Although continued cooperation between the CMS and SHM is necessary to fine-tune the measures, below are those that the SHM believes are reportable by, and most relevant to, hospitalists.
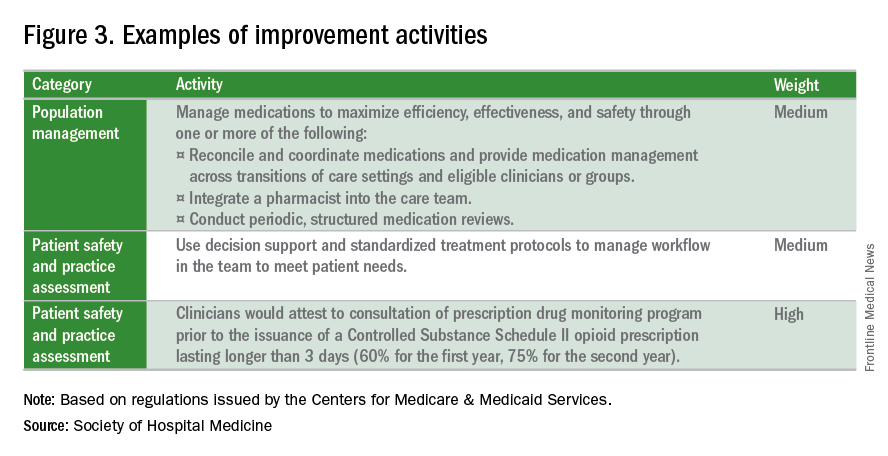
The improvement activities category will determine 15% of hospitalists’ performance in the MIPS. To receive full credit for this category, hospitalists must report on activities totaling 40 points. There are 92 available activities across eight different categories – 20 points for those that have a “high” weight determination and 10 points for those with medium weight.
In 2017, the CMS will calculate the cost category for providers, but it will not be counted toward the overall score. The data will still be collected based on Medicare Part A and Part B costs and will be reported to groups. Over time, this category will increase in scoring weight.
The Advancing Care Information category replaces the meaningful use program. This category will still promote EHR use, but hospitalists should be exempt from this category because of their “hospital-based” practice setting. This exemption is the reason why the quality category counts for 85% of the hospitalists’ score.
What is the APM Track?
The Alternative Payment Model pathway will be difficult for hospitalists to participate in, given its current criteria. Only advanced APMs will qualify, and for an APM to qualify as advanced, its clinicians/groups must use certified EHR technology, tie clinician payments to quality measures, and bear greater than nominal financial risk for outcomes and expenses, or qualify as a medical home. A provider must also meet rather high patient or payment thresholds coming from the model (greater than 25% of Medicare payments or greater than 20% of patients as part of an APM) in order to qualify.