Joint Commission Resource Educates Patients, Hospitalists about Antibiotics
The Joint Commission has launched a new online resource for patients and hospitalists to help change mindsets and start conversations about proper antibiotic usage.
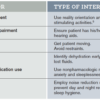
The SpeakUp: Antibiotics campaign is a package of free materials, including an infographic illustrating which illnesses may require an antibiotic, a list of questions for patients to ask when prescribed an antibiotic, a podcast, and a video reminding patients that antibiotics are not needed for colds or the flu.
“The new SpeakUp campaign provides a variety of resources to help patients and caregivers understand that how they use antibiotics today can affect how well the drugs work for them tomorrow,” says Lisa Waldowski, MS, APRN, CIC, infection control specialist at The Joint Commission.
The primary audience for these materials is the consumer, but hospitalists and healthcare workers are the crucial secondary audience. “This is a partnership; the knowledge needs to go both ways,” Waldowski says. “Sometimes there’s an expectation that when you see a physician, you are somehow shortchanged if you don’t leave with a prescription for an antibiotic.
There’s an education that needs to go on in the mindset of the physician, [in terms of] looking at whether this situation warrants an antibiotic and educating the patient if it does not. It takes time to have that conversation.”
The campaign can also provide a starting point for hospitalists to make changes in the workplace. “The information needs to be digested by everyone individually, but collectively in the organization where you work, this can lead to an antibiotic stewardship program, a coordinated intervention,” she says. She recommends a multidisciplinary approach. “Sometimes successful programs are led by a physician, and they have a strong pharmacy component, working together and supporting one another to use antibiotics appropriately.”