Escalate HIV adherence strategies amid COVID-19
“The writing is on the wall” that virtual care is not meeting the needs of people with HIV who struggled with viral suppression even before the COVID-19 pandemic, said Jason Farley, PhD, ANP-BC, AACRN, associate professor of nursing at Johns Hopkins University, Baltimore. So it’s time for HIV care teams, especially clinics in the Ryan White HIV/AIDS Program, to get creative in bringing wraparound services to patients.
That may mean reallocating the workforce so that one person serves as a community health worker. Or it could mean increasing texts and video calls; helping patients find online support groups to address problems with alcohol or drug use; and conducting an overall assessment of patients’ needs as the pandemic continues.
“The virtual patient-centered medical home may be the new normal after COVID-19, and we have to be thinking about how we use this model with patients for whom it works, but supplement this model in patients that it does not,” Farley said at the virtual Association of Nurses in AIDS Care (ANAC) 2020 Annual Meeting. That work “is essential to our being able to facilitate the best patient outcomes possible.”
Early data, tiered interventions
Farley referred to an article published in September in the Journal AIDS that confirmed unpublished data mentioned at the International AIDS Conference 2020. The article reported that viral suppression rates among people with HIV who attended San Francisco’s Ward 86 HIV clinic dropped by 31% from pre-COVID levels.
Of the 1766 people who attended the clinic, about 1 in 5 had detectable HIV viral loads at any point in 2019. But that rate was 31% higher after shelter-in-place orders were issued. And although patients participated in telemedicine visits at more or less the same rate before and after the pandemic (31% vs. 30% no-shows), viral suppression rates dropped. The impact was especially acute for homeless individuals.
“This destabilization occurred despite our population attending telemedicine visits at a higher rate than expected, given the 60% drop in ambulatory care visit volume nationwide,” the authors stated in their article. “Telehealth visits, while offering greater patient convenience, may lead to less access to clinic-based social support services essential to achieving viral suppression among vulnerable groups.”
That’s the challenge HIV clinics now face, Farley said at the ANAC meeting.
He suggested a differentiated care approach in which there are four tiers of care, starting with the standard level of outreach, which may include email, electronic health record blasts, and robo-calls to remind people of their appointments and to refill their medications. Those with sustained viral suppression may only need 90-day automatic refills of their medications. Those who are vulnerable to nonadherence may need to be contacted weekly or more often by the clinic. Such contact could be made by a social worker, a community health worker, or through some form of virtual support.
Patients at tier 4, who have labile viral suppression, need far more than that. These are the 15% of patients with HIV who struggled with viral suppression before the pandemic. They are the patients that Farley’s team focuses on at Baltimore’s John G. Bartlett Specialty Clinic for Infectious Disease.
“We’ve completely deconstructed the patient-centered medical home,” he said of the early move to virtual care. He suggested that clinicians assess their services and ask themselves some questions:
- Has someone on the team reached out to every patient and checked in to see what their biggest needs are, medical or not, during the pandemic? Have they assessed the patient’s ability to receive video calls or text messages?
- How have group-support programs that address stigma or the social determinants of health fared in the transition to virtual medicine?
- Are patients who are in recovery being supported in order that they may engage with recovery programs online?
- How well have counseling services done in engaging people in virtual care? Currently, given the overall increase in mental health challenges during the pandemic, one would expect that the use of mental health counseling is increasing. “If they’re stagnant or going down, someone needs to be reflecting on that issue internally in the clinic,” he said.
- Are patients being contacted regarding the effects that isolation is having on their lives? “The things that would normally allow us to self-mitigate and self-manage these conditions, like going to the gym, meeting with friends, religious services – all of those are being cut,” he said.
- Is there an early alert from an in-person pharmacy to trigger outreach via a community health worker for patients who haven’t picked up their medications in a week or more?
Farley pointed to a 2015 model for an enhanced e-health approach to chronic care management that called for e-support from the community and that was enhanced through virtual communities.
These are some of the approaches Farley has taken at his clinic. He leads a team that focuses specifically on patients who struggled with engagement before the pandemic. Through a grant from the US Department of Health & Human Services’ Health Resources and Services Administration – even before the pandemic – that team has been funding community health workers who have multiple contacts with patients online and virtually and are able to offer what he calls “unapologetically enabling” support for patients so that they are able to focus on their health.
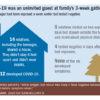
He gave the following example. Before the pandemic, a community health worker on the team had been working with a patient who showed up at every scheduled visit and swore that she was taking her medications, although clearly she was not. A community health worker, who was made available through the grant, was able to recognize that the patient’s biggest challenge in her life was providing childcare for her special-needs child. The community health worker worked with the patient for months to find stable childcare for the child, paid 2 months of rent for the patient so that she would not become homeless, and helped her find transitional housing. When the pandemic hit, the community health worker was already texting and conducting video calls with the patient regularly.
For the past 9 months, that patient has had an undetectable viral load, Farley said.
“Nine months during a pandemic,” Farley reiterated, “and the community health worker keeps working with her, keeps meeting with her.”