Case
A 45-year-old hospitalist, a familiar face in the system for the past decade, tragically took his own life. His colleagues and staff admired him, and he always had a pleasant working personality. However, he had been struggling lately. This bright and excellent physician went from being a well-respected clinician to being laid off. Who should we blame: The system? The workload? The toxic work environment? Job dissatisfaction? The clinician’s personality? Or something else?
In 2023, the nationwide clinician burnout rate exceeded 50% for physicians and advanced practice practitioners (APPs).1 Burnout costs the U.S. healthcare system roughly $5 billion annually due to reduced clinical productivity and increased physician turnover.2 So much so that the U.S. Surgeon General issued a 2023 advisory report raising the alarm on this public health risk. Burnout not only threatens the health and well-being of the individual clinicians impacted (physicians have the highest suicide rate of any profession) but also results in poorer quality of care for our patients. Physicians who are burnt out are twice as likely to commit a medical error.3 The link between burnout and errors is not confined to individuals at the extremes of the burnout spectrum; it’s a continuum.4
Burnout has led to early physician retirements and clinicians leaving the profession, resulting in an unprecedented physician shortage and access challenges. This jeopardizes our ability to meet the community’s needs and fulfill our mission of making healthcare more accessible to improve quality of life. The question is, how can we, as a healthcare system, tackle this issue head-on? The solution lies in collaboration. It’s not about finding the best solution, but rather working together to implement and foster a culture of collaboration to make a difference and empower our healthcare professionals.
CHIM
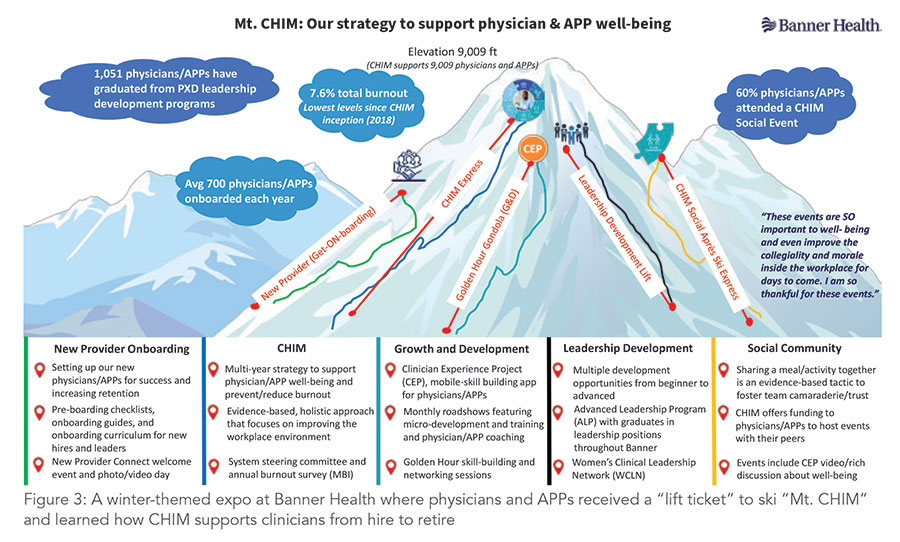
In 2019, before the COVID-19 pandemic hit, Banner Health began concerted efforts to promote well-being by introducing the Cultivating Happiness in Medicine (CHIM) strategy. We continued these efforts throughout the pandemic. Arizona was twice the world’s hottest hot spot for COVID-19, but we continued and extended well-being programs to physicians and APPs. This included encouraging social activities appropriately tailored to meet public health guidelines. This unwavering commitment to combat burnout during the most challenging times, alongside physicians and APPs, was a courageous step to combat the burnout crisis.
The CHIM strategy is a comprehensive, evidence-based approach, driven by clinicians, that supports wellness from an individual and organizational perspective. By engaging, inspiring, and empowering them to live their best day in medicine, connect with their purpose, and achieve their career goals through intentional growth and development, CHIM aims to usher in a positive transformation in the healthcare landscape. We believe engaging the team and asking for opinions is essential before starting such a significant initiative. Before launching any work, our Physician and APP Experience and Development Team conducts a listen, learn, plan, and act cycle to ensure we capture the clinician’s voice in our plans and activities.
Pillars of CHIM
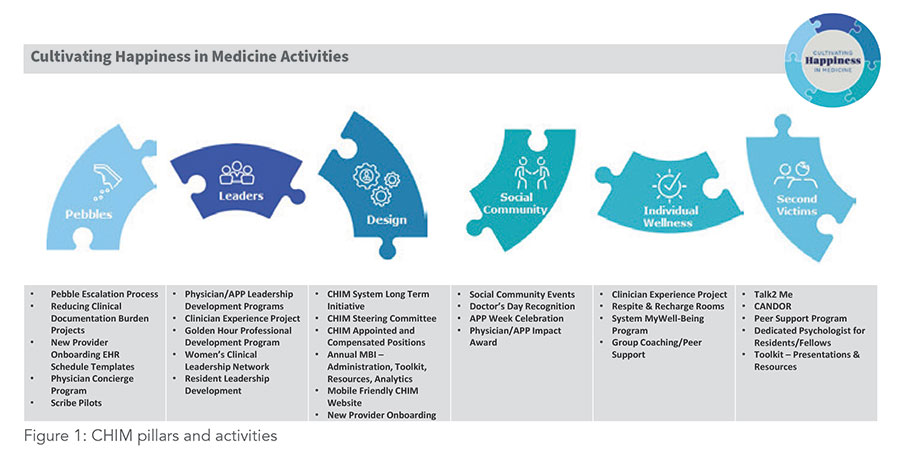
The CHIM strategy incorporates the Swensen Model to support wellness from a holistic, evidence-based perspective. The six dimensions of the strategy include the following (see Figure 1):
- Design: Creating organizational systems that address the human needs for meaning, purpose, and autonomy in work
- Leaders: Developing leaders who will collaborate and engage with physicians and APPs as trusted partners and practice participative management by involving them in problem-solving and decision making
- Social Community: Creating opportunities for physicians and APPs to build relationships with their colleagues and cultivate community and camaraderie
- Individual Wellness and Well-being: Promoting resources and programs that help physicians and APPs develop healthy habits such as mindfulness, resiliency, exercise, sleep, nutrition, mental and emotional health, and more
- Second Victims: Reducing preventable harm and supporting staff members involved with a preventable adverse patient event (second victims) by providing emotional and psychological support, addressing the root cause, and establishing a fair and just culture
- Pebbles: Removing sources of workflow, process, operational frustrations, and inefficiencies that act as the “pebble in your shoe”
Strategies in CHIM
The CHIM model uses various strategies. It is led by a system physician and APP steering committee to oversee our work and ensure we create valuable resources and effective tactics to support our clinicians. The strategies are discussed below.
1. Clinician Experience Project (CEP)
The CEP uses app-based video content that can contribute to excellence in healthcare.5 It uses a “micro-learning” approach in which clinicians spend five to 10 minutes per week learning practical coaching tips. Examples of topics include bringing cheerfulness to work, team positivity, effective communications among teams, end-of-life care, patient experience, partnering with a nurse, efficient rounding, quality and safety, value-based care, telehealth, conveying respect for each other as team members as well as patients, how to approach goals of care, and end-of-life discussions. These videos can also be shown in team meetings to engage the clinical team in learning and development. Figure 2 summarizes some of the common topics in CEP.
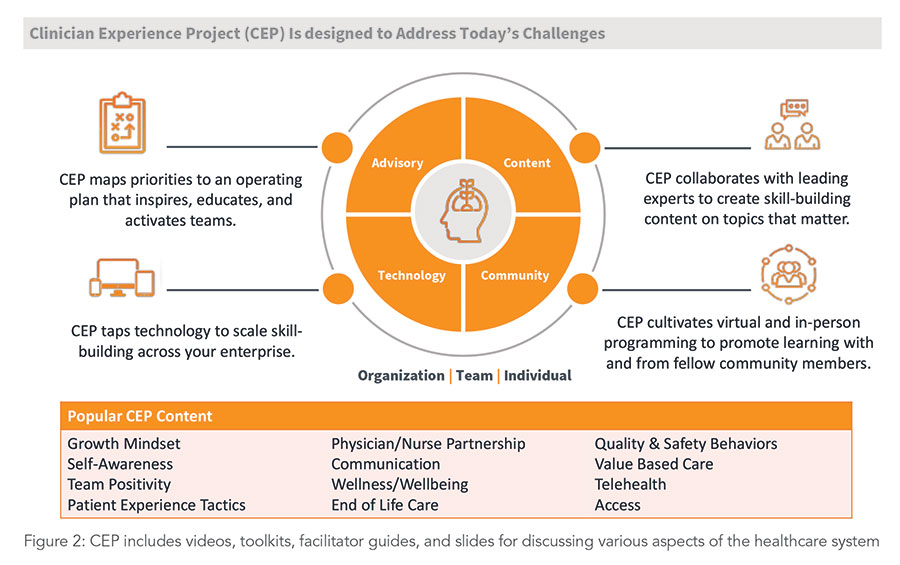
Clinicians can share insights with their colleagues by commenting on videos, collaborating with hospital leadership, and implementing effective organizational and policy changes. We have been using CEP since 2019. It has revolutionized patient care and improved healthcare workers’ mental well-being on issues that matter in daily patient care and workflow.
2. Professional development and leadership development programs
Evidence-based research shows that investing in a person’s personal and professional development can decrease burnout. We have been doing individual one-to-one clinician coaching, group coaching, self-guided virtual individual development, and a physician peer support program to encourage professional development. The goal is to offer a confidential, listening ear and support for physicians and APPs struggling with challenges. Additionally, we have a robust physician and APP leadership development program, with programs for those clinicians interested in leadership, first-time leaders, mid-level leaders (Leadership Development Program), resident leaders (Leadership Development for Residents), and advanced leaders through our Advanced Leadership Program.
3. New provider onboarding
Onboarding is critical in physician and APP retention, as practitioners with a good onboarding experience are more likely to stay for at least three years and are three times more likely to feel a solid commitment to their employer. We support the physician and APP from hire to retire, beginning with new provider onboarding, where we create a pre-boarding checklist and provide onboarding guides for each business line. This ensures a smooth start for new clinicians and equips them with the resources and support for success. We have a live, new provider, onboarding event to connect with essential stakeholders and resource teams and a warm welcome photo and video day.
4. Reward and recognition for our providers
We support and promote rewards and recognition for our practitioners and team members. Our MVP (Most Valuable People) program and the system’s annual Doctors’ Day and APP Week recognize, reward, and encourage team members who provide exceptional care. Our annual survey bundle comprises engagement, culture, safety, and burnout questions, taken anonymously by all stakeholders, that give open feedback about the health system, mentors, and organization leaders. These simple initiatives work immensely well to encourage a positive culture in the workplace. The aim is to build resilience in clinicians, reduce burnout, and allow them to bring their best selves to work.
5. CHIM social community events
Social community is one of the six pillars of the CHIM holistic, multi-faceted strategy. Sharing a meal is an evidence-based tactic that fosters community and improves team camaraderie, engagement, and trust. Moreover, it’s an opportunity for our clinicians to support one another as peers by sharing their experiences as providers with someone who’s been in similar situations and knows their challenges. We promote using social community events, a structured yet easy process for physicians and APPs to connect, share a meal or fun activity, access CHIM resources, and discuss well-being to support the social community pillar.
Since its inception in 2018, funding has been offered twice yearly, but more recently every quarter, to any Banner physician or APP willing to host a gathering of their peers, share a fun meal or activity, lead a CHIM discussion, and complete a simple registration form or post-event documentation process. Social Community improves team engagement and helps build relationships among team members. It is an opportunity for clinicians and leadership to support one another as peers by sharing their experiences as providers with someone who shares their challenges. We summarize all of this in Figure 3.
CHIM results
Burnout: The culmination of the CHIM and Physician and APP Experience and Development Team’s work resulted in a record-low 7.6% total burnout for physicians and APPs per a Maslach Burnout Inventory survey in 2023 (the lowest since CHIM’s inception in 2018 and well below the industry average of 9.9%). At Banner, we believe the business case for addressing physician burnout is multifaceted. It includes costs associated with turnover, lost revenue associated with decreased productivity, financial risk, and threats to the organization’s long-term viability due to the relationship between burnout and lower quality of care, decreased patient satisfaction, and problems with patient safety. As a result, reducing physician and APP burnout has significant, tangible results for the organization, our clinicians, and our patients. According to the latest estimates, our organization has saved $6.1 million in burnout reduction alone (not including reductions in turnover) since 2021.
Retention: Additionally, the collective CHIM activities in 2023 contributed to an improvement in physician retention and a reduction in physician and APP turnover from 2022 to 2023, resulting in an estimated organizational savings of $13 million. The 2023 CHIM spend was $625,000, which is less than the turnover cost of just one physician leaving the organization ($800,000), representing a monumental value added and return on investment.
CHIM social community events: Getting physicians to engage in any activity, let alone one that’s wholly voluntary, is challenging. In 2023, a record 60% of Banner physicians and APPs participated in a CHIM social community event, demonstrating that many physicians and APPs felt the CHIM social community events were a valuable use of their time. Furthermore, this means that more than 2,500 physicians and APPs enjoyed a fun activity, supported their wellness, and cultivated the happiness needed to reconnect them to their purpose and flourish in medicine. With the CHIM strategy, we’ve reduced burnout, increased engagement, and increased CEP usage among our team members.
Practicing and achieving excellence
As a result of our 2023 CHIM work, Banner Health was recognized as a 2023 American Medical Association Joy in Medicine organization. We believe we received this prestigious honor due to our investment in CHIM, which helped reduce burnout and achieve competencies in the AMA’s strict criteria, including burnout assessment, organizational and leadership commitment, efficiency of practice environment, and teamwork. Our work has captured both local and national attention. Other organizations have met with us to learn our best practices, and we’ve been featured nationally in presentations and leading publications.5 Locally, we’ve helped lead the way as a core organization member with the Well-Being Collaborative of Arizona, a group of 62 organizations across Arizona working collectively to improve the well-being of health professionals in our community. In 2023, our physicians and APPs told us they want to feel valued, appreciated, and connected to their purpose, and to have a sense of belonging, as in “I belong here.” This is how we can achieve excellence in health care and cultivate happiness in medicine.

Dr. Sood

Dr. Bessel
Dr. Sood is a hospitalist at Banner Gateway Medical Center in Gilbert, Ariz., affiliated with MD Anderson Cancer Center in Houston, Texas. Dr. Bessel is Banner Health’s chief clinical officer. She has a hospitalist background and was recently recognized as one of Modern Healthcare’s 50 most influential executives for 2024.
References
- Kane L. ‘I cry but no one cares’: Physician Burnout & Depression Report 2023. Medscape website. https://www.medscape.com/slideshow/2023-lifestyle-burnout-6016058. Published January 27, 2023. Accessed January 4, 2025.
- Yates SW. Physician stress and burnout. Am J Med. 2020;133(2):160-164. doi: 10.1016/j.amjmed.2019.08.034.
- Motluk A. Do doctors experiencing burnout make more errors? CMAJ. 2018;190(40):E1216-E1217. doi: 10.1503/cmaj.109-5663.
- Tawfik DS, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018;93(11):1571-80. doi: 10.1016/j.mayocp.2018.05.014.
- Sood, N. Practicing excellence in health care. Society of General Internal Medicine website. https://www.sgim.org/article/practicing-excellence-in-health-care/. Published July 2024. Accessed January 4, 2025.
CHIM social community events – Can you share what this looked like?