 A 75-year-old woman with a previous medical history of high blood pressure, diabetes mellitus, stage 4 chronic kidney disease, and lung cancer was admitted to the hospital with chest pain and shortness of breath at home. On an echocardiogram, she was found to have a pericardial effusion, which you think is from worsening malignancy. You treat her appropriately with cardiology on consult. You visit her in the afternoon after rounds to ask if she would want to talk about her goals of care, especially in the setting of this disease. After getting permission, you talk about code status and healthcare-power-of-attorney options while clarifying the state laws that apply if none is chosen. You document these findings in a note as a separate encounter and spend 40 minutes in this meeting.
A 75-year-old woman with a previous medical history of high blood pressure, diabetes mellitus, stage 4 chronic kidney disease, and lung cancer was admitted to the hospital with chest pain and shortness of breath at home. On an echocardiogram, she was found to have a pericardial effusion, which you think is from worsening malignancy. You treat her appropriately with cardiology on consult. You visit her in the afternoon after rounds to ask if she would want to talk about her goals of care, especially in the setting of this disease. After getting permission, you talk about code status and healthcare-power-of-attorney options while clarifying the state laws that apply if none is chosen. You document these findings in a note as a separate encounter and spend 40 minutes in this meeting.
What billing does this qualify for?
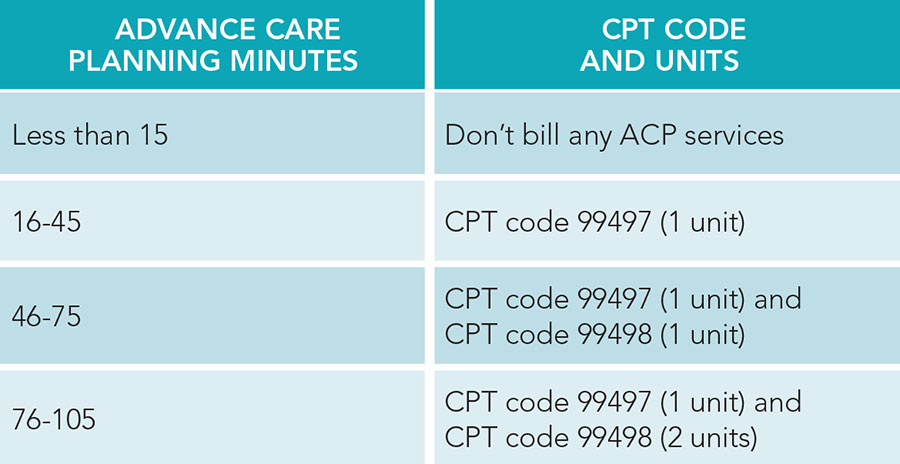 This can qualify for an advance care planning (ACP) billing code (99497). ACP includes the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified healthcare professional, face-to-face with the patient, family member(s), and/or surrogate. The first 30 minutes qualify for a 99497 code, while each additional 30 minutes qualify for a 99498 code.
This can qualify for an advance care planning (ACP) billing code (99497). ACP includes the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified healthcare professional, face-to-face with the patient, family member(s), and/or surrogate. The first 30 minutes qualify for a 99497 code, while each additional 30 minutes qualify for a 99498 code.
Here is a quick table to help you understand how to bill these by time. You must document the following for each visit:
- The voluntary nature of the visit
- The explanation of advance directives
- Who was present
- The time spent discussing ACP during the face-to-face encounter
- Any change in health status or healthcare wishes if the patient becomes unable to make their own decisions
Note: You cannot bill for ACP on a day that you bill 99291 (critical care service).
Dr. Mehta is the vice-chair of inpatient clinical affairs, medical director, and assistant professor of medicine in the clinical core faculty for program valuation and improvement at the University of Cincinnati Medical Center in Cincinnati.

