Once out of training, it sometimes becomes difficult to find formal instruction, especially in the realms of educating trainees while optimizing hospital throughput. One potential solution lies in peer observation programs, which allow for the development of skills within the workplace with real-time or immediate feedback. Drs. Margot E. Cohen, Ashok Linganna, Joyce Kim, and Andrew Orr implemented such a program and wrote a Brief Report titled “A novel hospitalist peer observation program to improve educational and operational rounding practices” published in the March 2024 issue of the Journal of Hospital Medicine (JHM). Concurrently, Drs. Lester Nixon and Sophia Gladding published a Perspective article titled “Peer observation to promote a culture of teaching and learning” in which they discussed the learning theory applied with peer observation. These two articles were the launchpad for our March #JHMChat.
We were joined by author Dr. Orr, who consolidated replies from his co-authors, and Dr. Nixon, representing himself and Dr. Gladding, and their valuable insight. As we discussed participants’ experience with peer observation, Dr. Orr discussed the reasoning behind the program: “We realized how little we all talked about our different rounding styles and how much we wanted to learn from each other.”
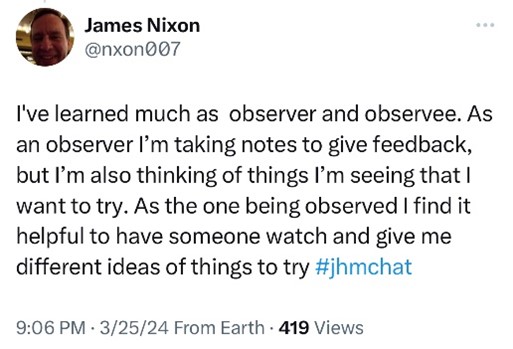
Dr. Nixon has learned just as much as both observer AND observee in this program, highlighting one of its key benefits.
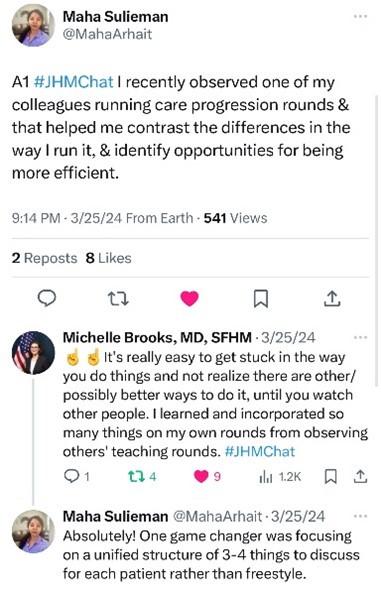
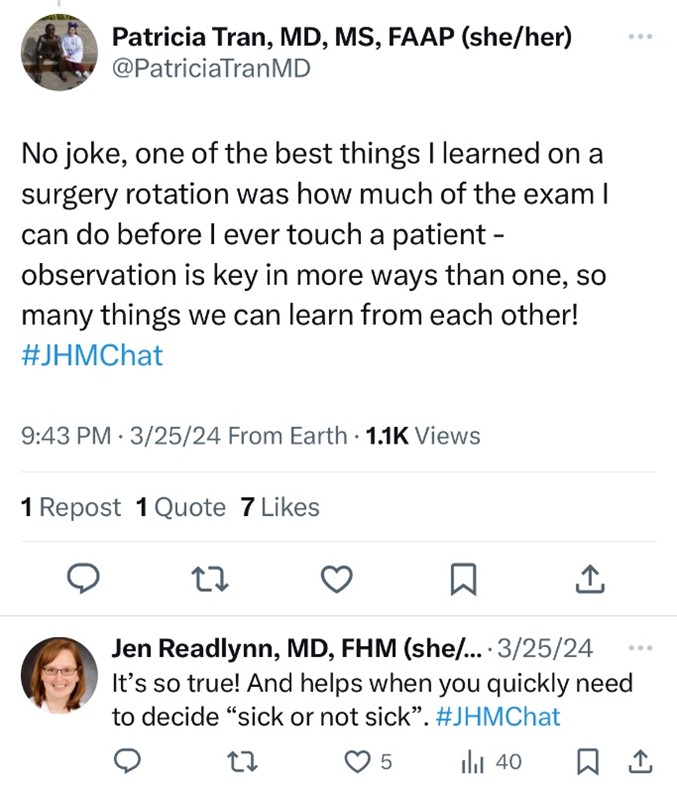
Dr. Maha Suleiman, JHM Digital Media Fellow, and Dr. Michelle Brooks (one of the JHM Digital Media Editors) discussed their own experiences with learning from others and identifying techniques and tricks to try in their own practice.
Others chimed in with what they would like their peer observation experience to highlight or focus on, such as time-saving (while maintaining value) measures and individual efficiency goals.
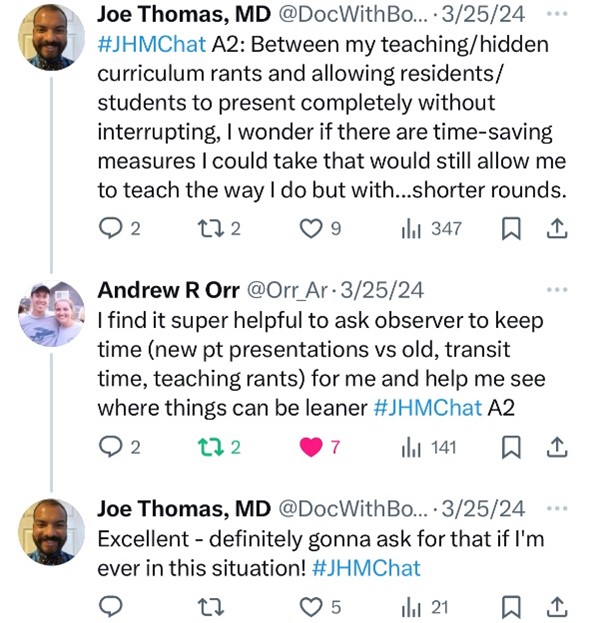
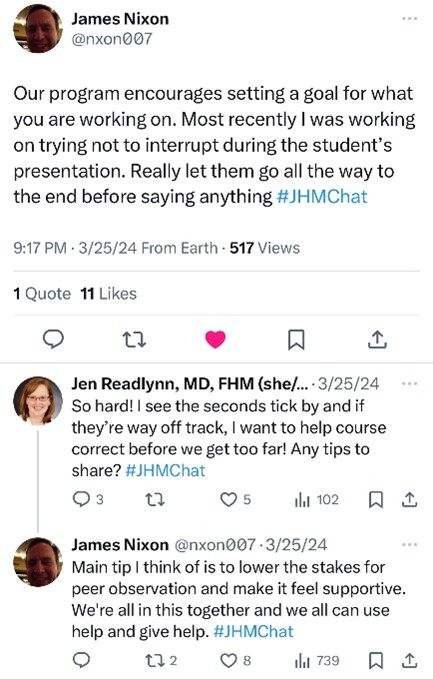
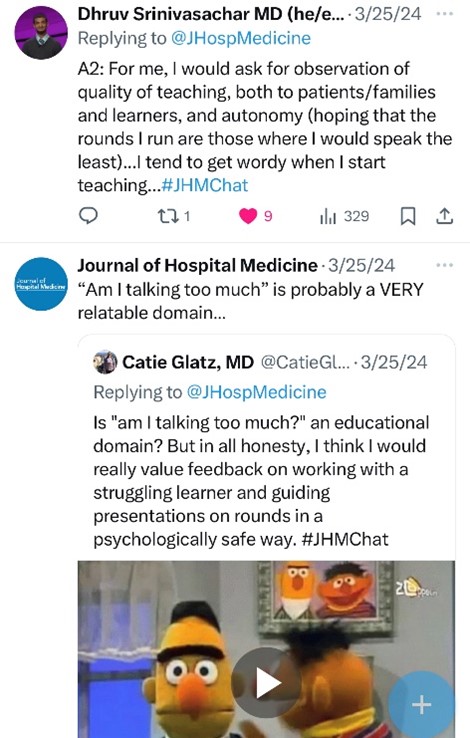
Apparently, we all wonder if we talk too much…
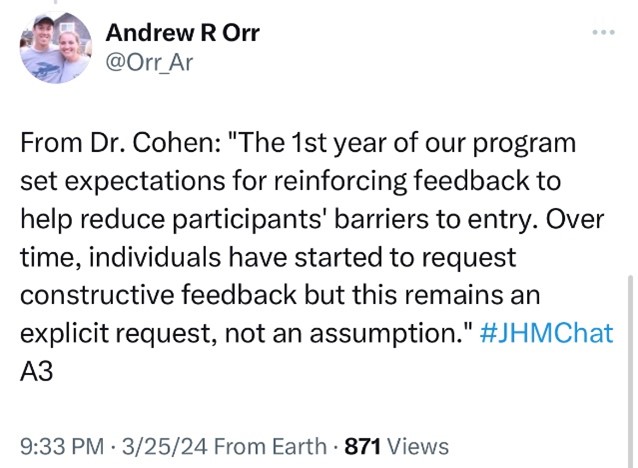
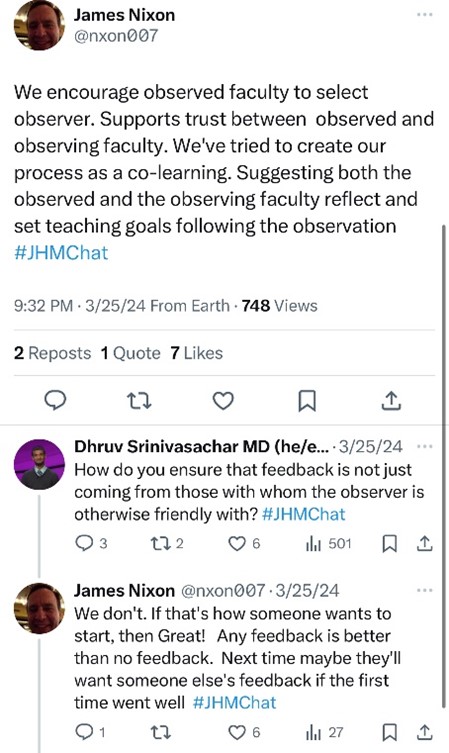
Peer Observation programs often pair junior and senior faculty, which can, unfortunately, suffer from hierarchical dynamics, which in turn suppress the learning environment. The Penn program worked to alleviate this by allowing observed hospitalists to choose their own observer, with success.
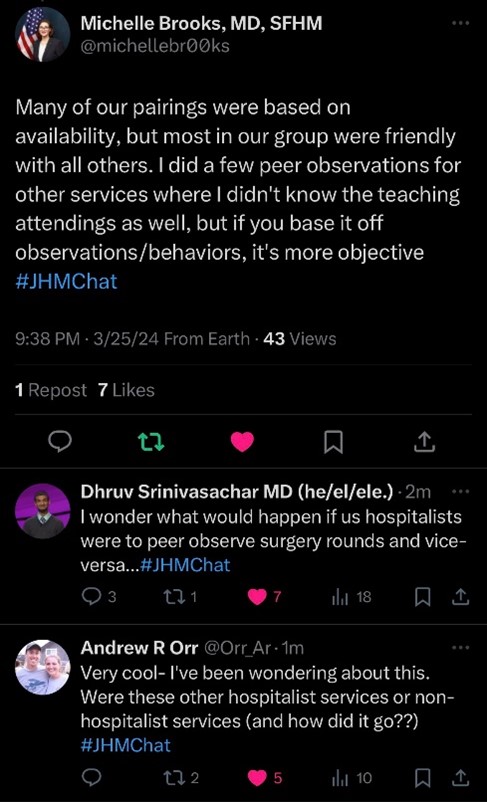
Taking it to the next level or looking to the future, the idea was raised to have hospitalists observe other services—not to give feedback, but to see what we could learn!
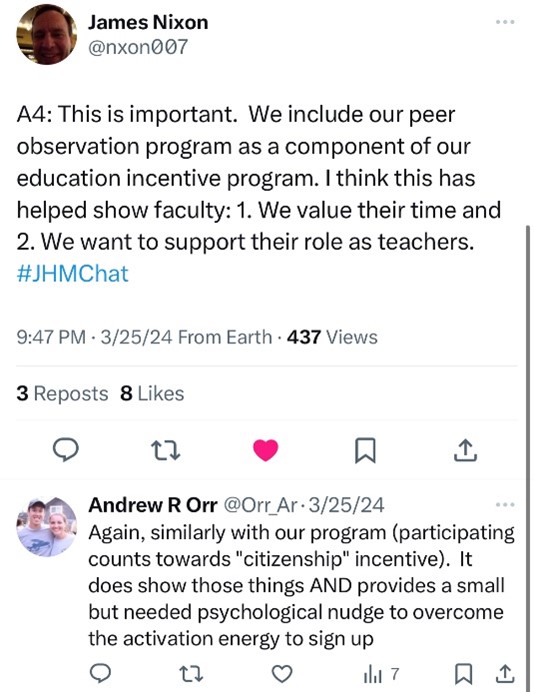
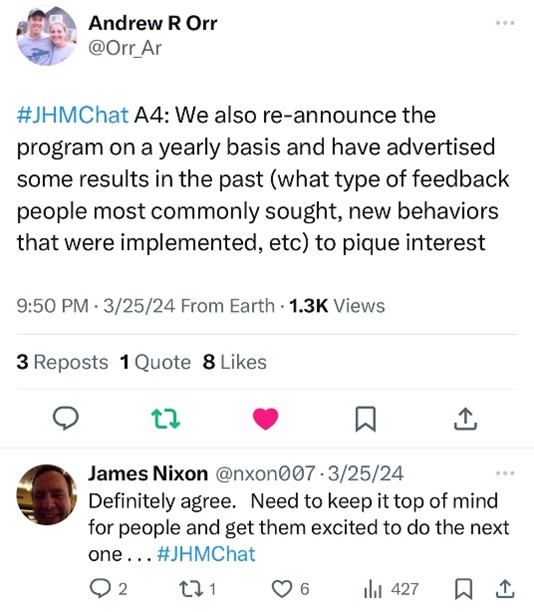
Finally, such programs cannot be successful without the retention and return of their participants. The authors emphasized that education and citizenship incentives, annual reminders of results and benefits, and emphasizing valuation of hospitalists’ time were key to success.
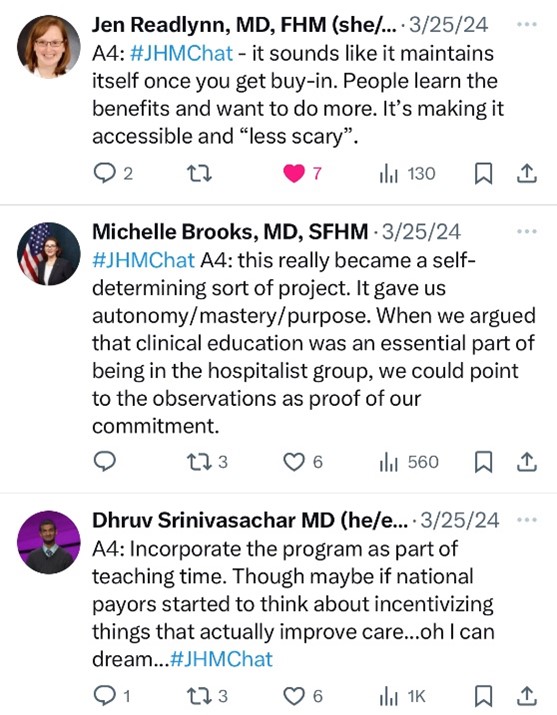
Dr. Brooks stated it succinctly: “What we do as teaching attendings is really difficult at times.” Still, we want to improve ourselves with increased efficiency and teaching prowess. Peer observation programs can be an excellent way for attending hospitalists to improve these domains in a real-time rounding environment, and hospitalists appreciate the value placed on their experience and time.
Please search #JHMChat to read these and more insightful posts, and we will see you at an upcoming #JHMChat! You can also read the full articles in the Journal of Hospital Medicine.
Dr. Thomas is a hospitalist with Buffalo Medical Group and clinical instructor with the community-based Catholic Health Internal Medicine Residency in Buffalo, N.Y. He is also a deputy editor, digital media for the Journal of Hospital Medicine.