Case
A 74-year-old frail man with diabetes mellitus, hypertension, and chronic kidney disease is admitted for severe community-acquired pneumonia. On hospital day four, the nurse reports a new sacral wound. Physical examination demonstrates a 3- by 4-cm oval wound on the sacrum that is pink and with partial-thickness skin loss. What is the best initial management of this suspected pressure injury (PI)?
Hospitalized patients have reduced mobility, which is the most critical risk factor for the development of a PI. In addition, inpatients have a host of other risk factors for hospital-acquired PI (HAPI), including advanced age, frailty, comorbid illness, decreased nutrition, and urinary and bowel incontinence. HAPIs negatively impact patient outcomes, increase length of stay, increase hospitalization costs, and can lead to pain, depression, and social isolation.1 Pressure injuries are significant health issues and a challenge to caregivers and the healthcare industry. The development of a severe PI is a life-changing sentinel event, and the Center for Medicare and Medicaid Services defines severe HAPI as “never events” and discontinues financial reimbursement when these originate in the hospital.
PIs have long been known to be a marker of poor overall prognosis. The development of a PI in the hospital increases the risk of mortality threefold, although this risk is largely due to the presence of severe coexisting medical comorbidities that likely contributed to the PI.2 Annually, it’s been estimated the cost of medical errors is over $17 billion, and PIs are the single most common type of medical error.3 Hospitalist physicians and advanced practice practitioners should be comfortable with the initial approach to a PI, given hospitalists, as first-line clinicians for many patients who develop PIs, have a significant role and responsibility for the prevention, detection, and treatment of PIs.
Management
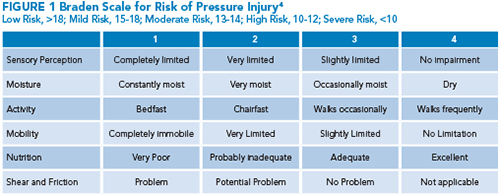
Before addressing the management of PIs, it should be emphasized that prevention is the critical first step for at-risk patients. The Braden scale (Figure 1) is the most widely used tool to assess PI risk. This scale consists of six risk categories including sensory perception, moisture, activity, mobility, nutrition, and friction or shear.4 Determining the level of risk can help identify the need for pressure-offloading intervention strategies to help prevent PIs.
 If a PI develops, hospitalists need to be comfortable performing the initial wound evaluation and staging. This begins by measuring the ulcer dimensions and evaluating the wound bed for the presence of granulation tissue, exudate, necrotic tissue, eschar, tunneling, or signs of infection.1
If a PI develops, hospitalists need to be comfortable performing the initial wound evaluation and staging. This begins by measuring the ulcer dimensions and evaluating the wound bed for the presence of granulation tissue, exudate, necrotic tissue, eschar, tunneling, or signs of infection.1
Signs of infection can be variable, but patients should be assessed for clues including systemic findings of sepsis such as fever, and localized findings of purulence, surrounding peri-wound erythema, warmth, tenderness, or foul-smelling discharge. Given the challenges in identifying infection in PI, especially in chronic PI, infectious disease consultation should be considered. When performing a PI evaluation, photographs entered into the electronic health record can be helpful for other care team members and monitoring.
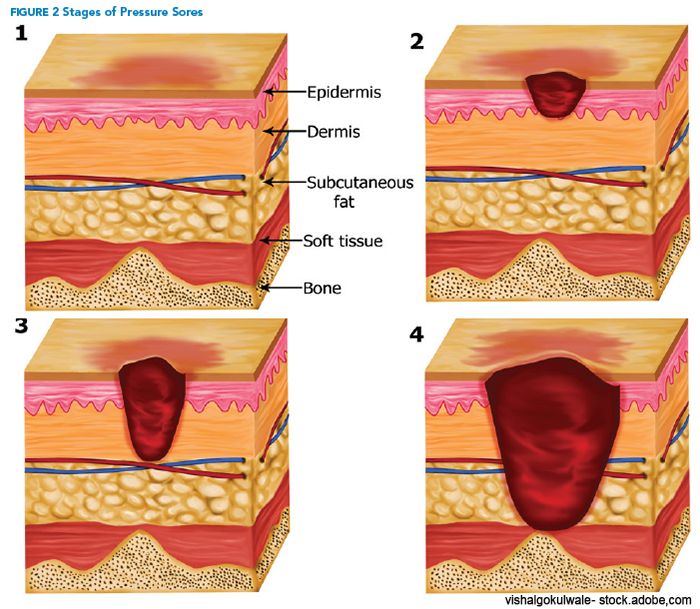 Staging is usually performed using the National Pressure Injury Advisory Panel staging system and is based on the initial wound appearance. Examples of the stages are shown in Figure 2. Stage 1 PIs have non-blanchable erythema with intact skin. Stage 2 PIs have partial-thickness skin loss with exposed dermis. Stage 3 PIs have full-thickness skin loss with adipose tissue visible. Stage 4 PIs have full-thickness skin and tissue loss with exposed fascia, muscle, tendon, ligament, cartilage, or bone. Some PIs may be unstageable if the wound bed is obscured by necrotic tissue, slough, or eschar. Deep-tissue PIs consist of persistent, non-blanchable, deep red, maroon, or purple discoloration, often with intact skin or a blood-filled blister.
Staging is usually performed using the National Pressure Injury Advisory Panel staging system and is based on the initial wound appearance. Examples of the stages are shown in Figure 2. Stage 1 PIs have non-blanchable erythema with intact skin. Stage 2 PIs have partial-thickness skin loss with exposed dermis. Stage 3 PIs have full-thickness skin loss with adipose tissue visible. Stage 4 PIs have full-thickness skin and tissue loss with exposed fascia, muscle, tendon, ligament, cartilage, or bone. Some PIs may be unstageable if the wound bed is obscured by necrotic tissue, slough, or eschar. Deep-tissue PIs consist of persistent, non-blanchable, deep red, maroon, or purple discoloration, often with intact skin or a blood-filled blister.
The treatment of PIs is complex and best performed with a multidisciplinary approach. The mainstays of treatment are addressing the etiology of the injury; pressure redistribution; debridement of non-viable necrotic tissue; maintaining a moist and clean wound-bed environment; and ensuring good nutrition.
In addition to the hospitalist, this often involves the patient’s primary nurse, a wound-care nurse specialist and/or a surgeon, a dietician, a physical therapist, and an occupational therapist. The overall medical condition of the patient should be assessed to determine the etiology of the wound as it is critical in wound healing to prevent further injury and address modifiable risk factors.
When initially evaluating possible PIs, hospitalists should consider other potential conditions that may be misdiagnosed as pressure-related, such as moisture-associated skin damage, abscess, burns, skin tears, inflammatory wounds, and malignancies such as squamous cell skin cancer. The clinical history of wound development often provides a clearer understanding of the cause.
There is a significant overlap between the prevention and treatment of pressure injuries, and patients with risk factors should be managed with pressure offloading on areas with the highest risk for injury, such as the sacrum, heel, and occiput. Hospitalists should monitor skin for medical device-related pressure injuries from oxygen tubing, nasal feeding tubes, and orthopedic devices.
Once a new wound is determined to be a PI, preventive strategies should be continued to minimize further skin breakdown. Patients should be frequently turned and repositioned, generally every two hours. Pressure support surfaces are designed to redistribute tissue load over a wider surface and ease pressure on bony prominences.5 These include specialty mattresses, integrated bed systems, and chair cushions. Advanced support surfaces are superior to regular hospital beds for managing pressure injuries.1 Trapeze bars can be used in a subset of patients to assist patients in repositioning themselves in bed.
Stage 1 PIs are typically covered for barrier protection, often with a foam dressing over pressure points.
For high-risk patients, foam dressings can also be used over bony prominences including the elbow, heel, sacrum, and occiput. For moisture control, skin-barrier zinc-based cream or no-sting barrier spray adds a layer of protection to the skin, especially if the patient has urinary or stool incontinence. Stage 2 PIs normally require little debridement. In addition to barrier protection and pressure offloading, stage 2 PIs are managed locally with an occlusive or semi-occlusive wound dressing that maintains a moist wound environment.5 Using moisturizing cream or ointment can help alleviate dry skin surrounding the wound.
Wound cleansing and debridement create a wound-bed environment optimal for healing. Wound cleansing is the process of using fluids to remove debris and microorganisms, and to provide better visualization to assess for potential debridement of necrotic tissue.5 Debridement is often required for stage 3 or 4 PIs. Debridement removes devitalized tissue, decreases barriers to wound healing, and potentially provides healing stimulatory effects.5 Adequate perfusion should be assessed before performing any debridement of the lower extremities. Debridement can be selective where only nonviable tissue is removed, or nonselective where both viable and nonviable tissues may be removed.
There are different methods of debridement. Autolytic debridement uses the body’s endogenous enzymes to loosen and liquefy necrotic tissue in the wound bed and is accomplished by using medical-grade Manuka honey, hydrocolloid, hydrogel, or films. Enzymatic or chemical debridement uses topical preparation of enzymes like collagenase (one common brand name is Santyl) that helps break down the devitalized collagen in the wound bed. Mechanical debridement is commonly accomplished with wet-to-dry dressing changes, where removing dried gauze acts as a debriding agent. Deep ulcers often require surgical debridement that can be performed at the bedside or in the operating room, in addition to packing deeper wounds. Other advanced therapies for deep ulcers are wound vacuum devices or skin grafting.
Other, general, care measures are important for all stages of wound healing. Good nutrition and hydration are essential, as patients with chronic PIs are in a catabolic state and often malnourished. When there is concern for inadequate oral intake, adding targeted nutrition therapy like nutritional supplements can support wound healing by enhancing collagen production. In addition, ensure patients are getting sufficient micronutrients and vitamins C, E, B12, and zinc to support the wound healing process. In addition to nutrition, physical and occupational therapy can encourage mobility and ambulation. Finally, remember PIs can be painful, debilitating, and life-altering for patients; thus, hospitalists should address our patients’ pain and offer psychosocial support.
PIs can lead to multiple clinical complications including wound infection, abscess, osteomyelitis, sepsis, and death. Infected PIs are one of the leading causes of infection in long-term care facilities.6 If a PI has extensive necrosis or is close to the anus, there is an increased risk of contamination with stool, and surgical procedures like debridement, diverting colostomy, and skin grafts may be required to effectively close the wound. Patients with larger or more complicated PIs may require care at long-term acute-care or skilled nursing facilities for wound management, thus increasing healthcare costs and further altering patients’ lives by keeping them from their home and their families.
Back to the case
This 74-year-old frail man developed a new sacral wound during his hospitalization that is consistent with a pressure injury. The pink sacral wound with partial-thickness skin loss is consistent with stage 2 PI. Initial wound evaluation should measure the size and depth of the wound, assess for necrotic tissue, and look for clues supporting infection such as purulence or foul-smelling discharge. A picture of the wound loaded into the electronic health record would be helpful for other clinicians and monitoring.
The initial management of the PI would first include addressing the etiology of the injury and implementing repositioning strategies to reduce further pressure injuries. Additional supportive measures should include a multidisciplinary care team that includes nurses, physical and occupational therapists, and a dietician. Care includes dressing changes to maintain a moist environment, optimizing nutrition, and increasing repositioning and mobility.
Bottom line
Management of PIs starts with individualized patient risk assessment, pressure offloading, provider comfort with early identification and staging, and a multidisciplinary care team.

Dr. Naidu

Dr. Hall

Dr. Gray
Dr. Naidu is an assistant professor in internal medicine, Dr. Hall is an associate professor in internal medicine and pediatrics, and Dr. Gray is an associate professor in internal medicine, all at the University of Kentucky in Lexington, Ky.
References
- Hajhosseini B, Longaker MT, et al. Pressure injury. Ann Surg. 2020;271(4):671-9.
- Berlowitz DR, Wilking SV. The short-term outcome of pressure sores. J Am Geriatr Soc. 1990;38(7):748-52.
- Van Den Bos J, Rustagi K, et al. The $17.1 billion problem: the annual cost of measurable medical errors. Health Aff (Millwood). 2011;30(4):596-603.
- Bergstrom N, Braden BJ, et al. The Braden scale for predicting pressure sore risk. Nurs Res. 1987;36(4):205-10.
- Kottner J, Cuddigan J, et al. Prevention and treatment of pressure ulcers/injuries: The protocol for the second update of the international clinical practice guideline 2019. J Tissue Viability. 2019;28(2):51-8.
- Garibaldi RA, Brodine S, et al. Infections among patients in nursing homes: policies, prevalence, problems. N Engl J Med. 1981;305(13):731-5.
Quiz
An 82-year-old man is hospitalized for a left femoral neck fracture after a fall. He undergoes operative repair on hospital day three and has a complicated hospital course with further debility and weakness resulting from traumatic rhabdomyolysis. One week into his hospital stay, the patient develops a sacral wound. The wound is 3 cm long, 2 cm wide, 1 cm deep, oval-shaped, and associated with full-thickness skin loss and exposed adipose tissue. No bone or other deeper tissue is seen. There is no surrounding erythema, purulence, necrosis, or eschar. Which of the following is the most likely stage of this pressure injury?
- Stage 1
- Stage 2
- Stage 3
- Stage 4
- Unstageable
Best Answer: 3. Hospitalists need to be comfortable performing the initial evaluation and staging of pressure injuries. This patient had risk factors for a pressure injury and was found to have full-thickness skin loss with exposed adipose tissue over his sacrum. This is most consistent with a stage 3 pressure injury.
Stage 1 pressure injuries have non-blanchable erythema of intact skin. Stage 2 pressure injuries have partial-thickness skin loss with exposed dermis. Stage 4 pressure injuries have full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone. Unstageable pressure injuries are obscured by necrotic tissue, slough, or eschar.
Key Takeaways
Hospitalists should assess for risk factors of PI and implement pressure-redistribution preventive strategies in high-risk patients.
Should a PI develop, hospitalists should perform proper initial wound evaluation including staging and evaluation for necrotic tissue or signs of infection.
Management involves a multidisciplinary team of nurses, a dietician, physical and occupational therapists, and often a wound care specialist.