Length of stay, work-relative value units, hospital-acquired infections.
There is no shortage of metrics—and their accompanying acronyms—that silo, summarize, and study whether hospitalists are doing their job. But perhaps the most ephemeral—and important—of those measurements is patient experience (PX).
That’s where SHM’s Patient Experience Special Interest Group steps in.

Dr. Mehta
“Having been the medical director of a 40-clinician hospitalist team, I understood earlier on the pain points about how patient experience is perceived in a very negative light,” said SIG chair Swati Mehta, MD, FACP, CPXP, SFHM. “And understandably so, because of how it has been framed historically as being just a data point we need to move. It’s a number. It’s a metric, rather than the right thing to do. Historically, the frame of reference is not a thing I was a fan of, and I wanted to change it. I wanted to find a way to find best practices to network and to understand better than what’s just happening with my own site.

Dr. Colella
“My passion for patient experience comes from believing it’s the heart of healthcare,” said SIG vice chair Jennifer Colella, MD, FACP. “It’s greater than the sum of the parts. One bad experience can taint even the best efforts to provide sterling care. Patients are unique with different experiences, expectations, and needs. Patient experience is an integral part of patient satisfaction, loyalty, and success for the entire healthcare system.
“Continued capture of market share depends on academic excellence, state-of-the-art facilities, proven continuing advancement in patient outcomes, or mitigation of suffering. Commitment to patient and family support by exceptional people directly and indirectly involved in patient care is a must. There is no substitute for a cohesive team that puts the patient first and shows that they care holistically to make every hospital admission the most positive experience possible with efficient and effective appropriate disposition and follow-up. Meeting and exceeding expectations is a cornerstone of success for everyone.”
Dr. Swati, national director of quality and performance for patient experience at Vituity and chair of SHM’s Patient Experience Executive Council, says one of the challenges of improving patient experience is getting hospitalists and others to move beyond seeing it as ticking off a measurement box, and to focus on actually improving a patient’s experience in the hospital.
“For the nerds in us, most docs are science-driven, right? That’s why we went to med school,” she said. “We want to learn the data behind it. We want to know this is the right thing to do, and not just a metric.”
So Dr. Swati points to what she calls the “why behind it,” which has three main pillars.
First, she said, “When we compassionately sit down and communicate better with our patients, study after study has shown that patients adhere more to their medications, their clinical outcomes improve, and they come back less often for unnecessary readmissions, and they really take better care of themselves because they feel like their doc really cares for them.”
Second, a better patient experience makes for a better hospitalist experience.
“Honestly, it’s a very selfish move to be selfless with patients and to really care for our patients,” Dr. Swati said. “We get a kick in our step after a good interaction. We feel good. We feel pumped even if we have five more admissions, we’ll take them on because we just had a good interaction. Knowing very well that the [reverse] is also true…poor interactions can really deflate us. This is the what and why for me.”
The third motivation is financial, personal, and professional.
“If you want to stay in the community you are in, if you don’t want to move, we need job stability, we need security, and we need to really think about not just our clinical role as a hospitalist, but how can I make sure my hospital’s doors are always open?” Dr. Swati said. “That’s all about patient loyalty. Patient’s word of mouth. They come back (and say) ‘Yes, I recommend this hospital,’ and we are going to thrive in our community.”
Dr. Colella, medical director of patient experience at Nebraska Medical Center in Omaha, says it would be “folly to trivialize any aspect of the patient’s experience.”
“Patient experience encompasses the totality of care,” she said. “It ties together all the components that go into a successful healthcare system from the patient’s perspective. You cannot have a first-class hospital system without patients recognizing the importance of every contact at every level over time. This includes everyone at our facility. Interpersonal relations are part of the patient’s experience, and all components are necessary. All healthcare is a continuum and continuous improvement based upon metrics that are deemed necessary and appropriate will be an ongoing endeavor.”
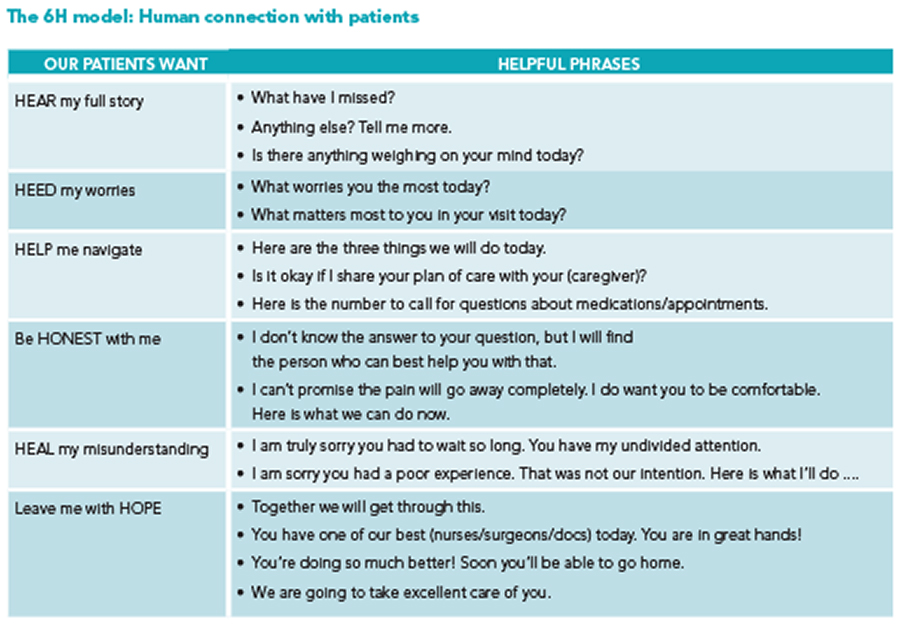
Dr. Swati boils patient experience down to the 6H model and the three Cs, which is what she highlights whenever she makes presentations on the topic: culture, connect, and correct. Building a team-based approach that values the patient’s experience, connecting with them to make them see that, and then correcting inevitable mistakes.
“Things are going to go south,” Dr. Swati said. “Patients will be in the room for too long. Patients will be waiting too long. They got the wrong medicine. Things will happen in life, just like in healthcare, but how do we correct issues? How do we apologize immediately? How do we do that recovery to gain the patient’s loyalty and forgiveness? If you focus on culture, connection, and correction, I think those are good standards to continue PX.”
Richard Quinn is a freelance writer in New Jersey.