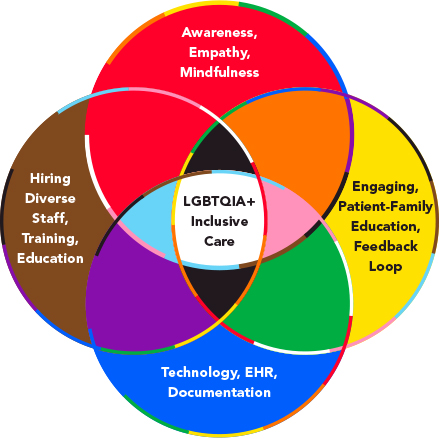
LGBTQIA+ Inclusive Care Venn Diagram
Our first and foremost duty in healthcare is to provide our patients with compassionate and equitable care. Members of the lesbian, gay, bisexual, transgender, queer or questioning, intersex, and asexual (LGBTQIA+) community often face significant barriers within the healthcare system. Our duty as healthcare practitioners and leaders of healthcare institutions is to address these issues and work toward inclusivity.
Over the years, we have heard heartbreaking stories about the experiences of LGBTQIA+ patients with healthcare providers.1 LGBTQIA+ individuals often face unique healthcare needs that clinicians overlook due to education gaps and discrimination.2 These include improper identification, dismissiveness of gender-identity roles, discrimination with treatment options, and many more. Additionally, the community also exhibits higher rates of substance abuse, suicide, promiscuous sexual behaviors, behavioral health issues, and self-harm.3
These issues illustrate the urgency of taking action to improve inclusive healthcare provision and rectify systemic flaws. In response, we initiated a collaborative project to develop a Gender Inclusive Care Toolkit for Hospitals.4 We did this by conducting a rigorous examination of medical journals and interviewing patients and clinicians representing the LGBTQIA+ community to understand how we could better meet the care needs of our patients. We consolidated those insights into resources that could easily be adapted for use in institutions from large academic medical centers to community hospitals and local practices. By tackling these important concerns and offering feasible solutions, we aim to help more healthcare settings provide fairer and more equitable care to everyone.
Despite advances in legal protections and acceptance of the community, there have been barriers to LGBTQIA+ patients receiving equitable and inclusive healthcare. Evidence indicates that LGBTQIA+ individuals are more likely to use tobacco than cisgender heterosexual adults and sexual minority women have been reported as having higher BMI than their heterosexual counterparts.5
The toolkit offers a host of resources and guidelines designed to increase awareness of innate biases. The toolkit also provides valuable resources on healthcare disparities experienced by LGBTQIA+ people, equipping healthcare practitioners with knowledge on recognizing and mitigating unconscious biases to provide compassionate, respectful, culturally competent care. With the toolkit, the goal was to equip healthcare staff with tools for identifying and combating unconscious biases that may negatively impact patient care by providing information on healthcare disparities, collaborating with organizations for resources, and increasing the training we provide medical and nursing students so that LGBTQIA+ care becomes an essential part of their studies.
Here are a few salient points from the toolkit:
- Empathy and mindfulness can serve as the cornerstones of building trust with patients. Hospitalists working with LGBTQIA+ patients should adopt an inclusive mindset, employ culturally sensitive terminology, and practice active listening. This ensures a nonjudgmental atmosphere that protects privacy while simultaneously creating space for open and honest communications.
- Technology can play an invaluable role in providing better healthcare to members of the LGBTQIA+ community. Electronic health records (EHRs) provide us with a powerful ally in this effort by ensuring the “sexual orientation” and “gender identity” data fields are always readily available within healthcare systems. Every visit is reviewed to ensure EHR entries are culturally sensitive; this allows every aspect of care provided for LGBTQIA+ patients to be tailored specifically.
- Culture-competent healthcare requires meaningful patient engagement throughout the hospitalization. Our aim at every step should be to include patients and family members during their healthcare journey, building open relationships between hospitalist and patient with empathic communication and trust among clinicians and patients alike. Respecting the identities of our patients and using preferred pronouns are powerful yet simple gestures of inclusion that demonstrate our dedication.
- Communication and feedback loops are vital for continuous improvement. By conducting patient-satisfaction and process-improvement surveys after every encounter, we gain invaluable insight into strengths and growth opportunities. Sharing these results with healthcare professionals and administrators promotes accountability while quickly addressing any deficiencies or weaknesses.
- Diversity is not only a goal but also a necessity in the healthcare workforce. We enrich our institutions by actively recruiting and supporting LGBTQIA+ employees. Building trust and communication channels between healthcare professionals and patients is crucial to creating an environment where everyone feels understood and valued.
- Education is at the core of our strategy to reduce healthcare disparities experienced by LGBTQIA+ people. By including training on bias against this community in medical and nursing curricula, future generations will possess the knowledge and skills to provide equal care for everyone. And developing bias-reduction skills among students is vital in creating more inclusive healthcare environments.
This toolkit features practical measures designed to increase empathy and mindfulness among healthcare providers, use technology to better care for LGBTQIA+ patients, include families and patients in decision-making, implement feedback loops and closed communication for continuous improvement, as well as increase diversity within the healthcare workforce. By employing the above measures within their institutions, hospitals can foster more inclusivity in the workplace. Even simple educational techniques, such as attending training sessions on using inclusive language and practices with patients and advocating for institutional resources and support, can create environments where LGBTQIA+ people feel valued, respected, and understood.
LGBTQIA+ patients experience various mental health challenges that include emotional distress, stigmatization, victimization, discrimination, and barriers to healthcare services.6 Although LGBTQIA+ rights have been legalized across numerous nations; they still experience significant mental health challenges that require further attention. The Gender Inclusive Care Toolkit for Hospitals is an important and tangible step toward addressing healthcare disparities and promoting LGBTQIA+ inclusive care. Hospitalists can play an essential role in creating healthcare environments that empower and respect all people through increased awareness of bias, improved patient engagement, technology advances, and commitments to diversity education and training. There is something special and comforting about being part of something bigger, and being around other like-minded individuals who empathize with other communities and groups. Our toolkit can promote this positive culture in a stressful setting and thus significantly improve patient satisfaction.

Dr. Dhillon
Dr. Grewal

Dr. Buddhavarapu

Dr. Munjal

Dr. Kashyap
Dr. Dhillon is an assistant medical director at Adfinitas Health in Hanover, Md., and an adjunct assistant professor and hospitalist at the University of Maryland Baltimore Washington Medical Center in Glen Burnie, Md. Dr. Grewal is a radiologist and an assistant professor at Florida State University College of Medicine in Pensacola, Fla. Dr. Buddhavarapu is a hospitalist at Banner Health’s Banner Baywood Medicine Center, Banner Health, in Mesa, Ariz. Dr. Munjal is an adjunct assistant professor in the department of nephrology at Touro University College of Osteopathic Medicine in Vallejo, Calif. Dr. Kashyap is the medical director research at WellSpan Health in York, Pa., and assistant professor of anesthesiology at the Mayo Clinic in Rochester, Minn.
SHM’s CME in LGBTQIA+ Health
SHM offers continuing medical education (CME) content (free for members) developed by the LGBTQIA+ Task Force of the SHM Education Committee.
This series is geared toward physicians, nurse practitioners, and physician assistants practicing hospital medicine.
Objectives include:
- Recognize LGBTQ+ as a social determinant of health.
- Document using language that is consistent with the patient’s sexual orientation and gender identity.
- Recognize that risk scoring systems and laboratory reference ranges are not validated for transgender patients.
- Described the risk of abruptly stopping gender-affirming hormone therapy.
- Describe best practices for pre-exposure prophylaxis (PreP) therapy while patients are admitted to the hospital.
- Identify methods to advocate for LGBTQ+ patients.
- Apply methods for discussing gender identity, organ inventory, and sexual orientation with patients.
- Courses include:
- LGBTQ+ Affirming Language and Documentation
- Inpatient Care of Transgender Individuals: Gender Affirming Hormone Therapy
- LGBTQ+ as a Social Determinant of Health
- Advocacy for/with LGBTQ+ Persons: Population and Policy
- PrEP 101: A Hospitalist’s Guide to HIV Pre-Exposure Prophylaxis
References:
- Morris M, et al. Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC Med Educ. 2019;19(1):325.
- Moran CI. LGBTQ population health policy advocacy. Educ Health (Abingdon). 2021;34(1):19-21.
- Medina-Martínez J, et al. Health inequities in LGBT people and nursing interventions to reduce them: a systematic review. Int J Environ Res Public Health. 2021;18(22):11801.
- Dhillon G, et al. Gender inclusive care toolkit for hospitals. Lancet Reg Health Am. 2023;26:100583.
- Bass B, Nagy H. Cultural competence in the care of LGBTQ patients. 2023. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. PMID: 33085323.
- Moagi MM, et al. Mental health challenges of lesbian, gay, bisexual and transgender people: An integrated literature review. Health SA. 2021;26:1487.
I love everything about this article. thank you!