The physician advisor role has been evolving in adult medicine for many years. Hospitalists are well suited for this role given their broad knowledge base regarding health care systems and their innate ability to collaborate with multiple disciplines in a complex medical system. Despite this, investment in this role in pediatric hospital systems is far less common and represents missed opportunities for improving hospital reimbursement, limiting capacity restraints, and ensuring regulatory compliance, all while maintaining high-value care delivery.
Children’s Health System of Texas operates 562 pediatric beds in two acute-care hospitals in north Texas with approximately 17,199 discharges in 2022. The primary location is a quaternary care, free-standing, 490-bed children’s hospital in Dallas and the secondary location is a 72-bed children’s hospital in Plano, Texas. The system is affiliated with the University of Texas Southwestern Medical Center (UT Southwestern). Hospital bed types include medical/surgical, neonatal, cardiac, pediatric intensive care, and psychiatric beds.
Before 2020, the hospital system had limited physician leadership within the utilization management (UM) department. The hospital system, like many other health systems, contracted with a third-party vendor to determine the medical necessity of care, patient status (observation or inpatient), and denials management through peer-to-peer calls with insurance companies for hospitalized patients. Although this allowed primary attending physicians the ability to focus on direct patient care, third-party vendors have certain limitations. These limitations include only partial access to a health system’s electronic health records, no access to the primary medical team, lack of understanding of the intricacies of the health system, inability to identify payer or hospital denial trends and thus initiate change, and a significant gap in pediatric-specific expertise in supporting UM at a large health system.
In early 2020, the health system’s administration partnered with UT Southwestern’s division of pediatric hospital medicine (PHM) and department of pediatrics to start a novel pediatric hospitalist-led physician advisor program with the following goals:
- Review medical necessity of care for the health system
- Improve denials management through a robust peer-to-peer and appeals program
- Develop a fellowship elective to train PHM fellows about UM
Within 15 months, the hospitalist-physician advisor peer-to-peer role had an approval rate of 70% compared to 35% for the contracted third-party vendor. This success led to the program’s expansion with three additional pediatric-hospitalist faculty with dedicated time. All four physician advisors continued their clinical practice as pediatric hospitalists, which was crucial to the program’s collaborative success. Given their deep knowledge of health systems and peer-to-peer processes and their ability to collaborate with multiple specialties, pediatric hospitalists were well-positioned to excel in this role. With a broad scope of pediatric-specific knowledge and expertise in caring for children with medical complexity, and as natural problem solvers and change advocates, pediatric hospitalists in these crucial roles gave a significant advantage to the program.
In the last two years, the program has grown significantly in peer-to-peer, appeals, prior authorization management, and scholarly activity with fellowship-curriculum development.
Peer-to-peer
The program excelled in peer-to-peer communication and denials management. Following admission to a hospital bed, UM nurses, from both the hospital system and the payer, review documentation to support the medical necessity of care ordered by the treating physician. Following this review, the cases may be evaluated by the payer’s medical director and, if there is disagreement on the medical necessity of care, a peer-to-peer is often offered.
The peer-to-peer opportunity is arguably the least time-consuming yet highest-value step of the denials and appeals process with payers. However, the administrative time for scheduling and completing these discussions by the treating physician is tremendously burdensome. For this reason, many health systems contract with a third-party vendor to complete these discussions., This is financially restrictive as third-party vendors often require a monthly case limit or charge a per-diem rate per case. An internal program, supported by dedicated physician time, allowed all peer-to-peer opportunities to be explored.
With an internal program, the physician advisor communicates with the primary medical team for clarification of the clinical course, accesses the entirety of the medical record, and provides additional explanations to the medical directors of the insurance plan. The physician advisors are experts in pediatric hospital-based care and trained in the application of evidence-based guidelines (e.g., MCG and InterQual) used by payers. These skill sets allowed for a comprehensive discussion of the clinical case that’s often lost in the written appeal.
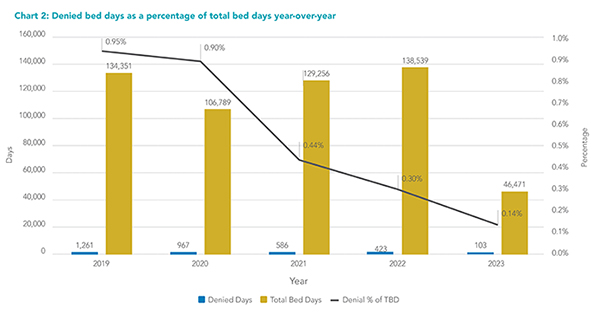
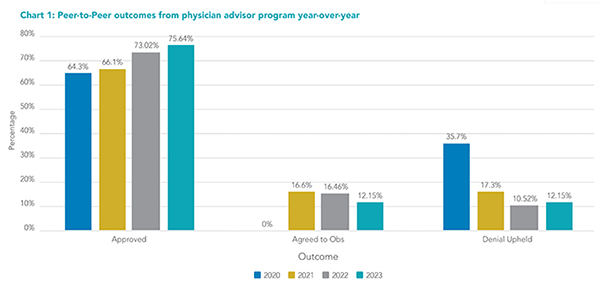 Full-time coverage for peer-to-peer support allowed the hospital system to take advantage of every opportunity to overturn a decision before moving forward with the administratively burdensome written appeal process. The physician advisor program achieved a denial overturn rate of 75% of peer-to-peers, leading to significant cost savings for the hospital system (see Chart 1). The percentage of denied bed days over total bed days significantly decreased (see Chart 2). Our internal program not only doubled the overturn rate compared to that of the vendor, but it also increased the volume of completed peer-to-peers from approximately 250 annually to nearly 700 in the program’s first year.
Full-time coverage for peer-to-peer support allowed the hospital system to take advantage of every opportunity to overturn a decision before moving forward with the administratively burdensome written appeal process. The physician advisor program achieved a denial overturn rate of 75% of peer-to-peers, leading to significant cost savings for the hospital system (see Chart 1). The percentage of denied bed days over total bed days significantly decreased (see Chart 2). Our internal program not only doubled the overturn rate compared to that of the vendor, but it also increased the volume of completed peer-to-peers from approximately 250 annually to nearly 700 in the program’s first year.
 Physician advisors act as liaisons between the hospital system, its physicians, and the payers. They attend division meetings of multiple specialties to educate both medical and surgical specialties regarding denial trends, opportunities for documentation improvement, addressing barriers to discharge, and opportunities to improve patient flow. While the administrative burden of completing the peer-to-peer is directed to the physician advisor, detailed feedback can be easily provided to the primary team and health-system leaders if needed. Additionally, the physician advisor is able to identify denial trends of specific payers and develop relationships with the payer’s medical directors to address these outside of the peer-to-peer process. This mechanism of bi-directional feedback illustrates the value of an internal program.
Physician advisors act as liaisons between the hospital system, its physicians, and the payers. They attend division meetings of multiple specialties to educate both medical and surgical specialties regarding denial trends, opportunities for documentation improvement, addressing barriers to discharge, and opportunities to improve patient flow. While the administrative burden of completing the peer-to-peer is directed to the physician advisor, detailed feedback can be easily provided to the primary team and health-system leaders if needed. Additionally, the physician advisor is able to identify denial trends of specific payers and develop relationships with the payer’s medical directors to address these outside of the peer-to-peer process. This mechanism of bi-directional feedback illustrates the value of an internal program.
Appeals management
If a peer-to-peer is unsuccessful, a written appeal may be submitted on the patient’s behalf. Due to the physician advisors’ increased approval rate in peer-to-peers, the volume of required written appeals significantly decreased, further minimizing the administrative burden of the appeals process. On the occasion of an unsuccessful peer-to-peer, the physician advisor, being intimately familiar with the case and the specific criteria applied by the payer, completed the written appeal in collaboration with the hospital’s denial-prevention department. Hospital collaboration with the physician advisor program in each step of the review and appeals process nearly eliminated the hospital system’s write-offs for medical necessity and status conflict by 2022.
Furthermore, certain high-cost medications such as inhaled nitric oxide are often denied by payers if administered outside of specific criteria set forth by payer policies. The physician advisor program created an appeal process for inhaled nitric oxide used in postoperative pediatric cardiac patients and has overturned denials for more than 650 days of nitric oxide usage in the last two and half years.
Prior authorization management
As the program grew in scope, it identified opportunities to improve prior-authorization processes with peer-to-peer support of planned admissions and surgeries. Health plans require prior authorizations for certain procedures, medications, or other services. If the prior-authorization request is denied, the payer offers a peer-to-peer. Again, the physician advisors’ expertise on medical necessity criteria used by payers ensures the appropriate prior-authorization request is made and can be further discussed peer-to-peer before the patient’s admission or procedure. Physician advisor involvement in this area ensures adherence to compliance regulations while maintaining appropriate reimbursement for the health system.
Scholarship
As part of UT Southwestern’s academic mission, the physician advisors developed a scholarship structure with an educational curriculum to teach trainees in the PHM division about UM basics including clinical documentation, managing peer-to-peer conversations using evidenced-based medical necessity guidelines, and hospital billing and reimbursement models. Currently, PHM fellows rotate through this elective, but the program anticipates growth into other subspecialties in the future.
A dedicated physician advisor program allows physicians to gain a robust understanding of payer and hospital trends, regulatory compliance, and medical necessity as defined by payers. Within a rapidly changing health care landscape, this knowledge can further drive performance improvement within the system. An internal program educates physicians and physicians-in-training to become better financial stewards of resource utilization within the health care system, which can directly impact the quality of patient care. Developing relationships with medical directors within the insurance plans and internal physician advisors allows a partnership in navigating the complexities of the health care system in an increasingly complex pediatric-patient population. The program’s ongoing growth and success highlight the importance of hospital and physician alignment in the need for improving patient care.
Physician participation is essential in improving the value of care at a system level and pediatric hospitalists can lead the change.

Dr. Johnson

Ms. Barraza

Ms. Landon

Dr. Mittal
Dr. Johnson is a pediatric hospitalist in the division of pediatric hospital medicine at the University of Texas Southwestern Medical Center, and medical director of utilization management for the Children’s Health System of Texas, both in Dallas. Ms. Barraza is vice president of centralized medication authorization and utilization management at Children’s Health System of Texas in Dallas. Ms. Landon is the senior vice president of managed care for the Children’s Health System of Texas and executive advisor for the new pediatric campus in Dallas. Dr. Mittal (@VMittalMDMBA) is a professor and division chief of pediatrics and program director of the PHM fellowship program at the University of Texas Southwestern Medical Center and Children’s Health System of Texas in Dallas.