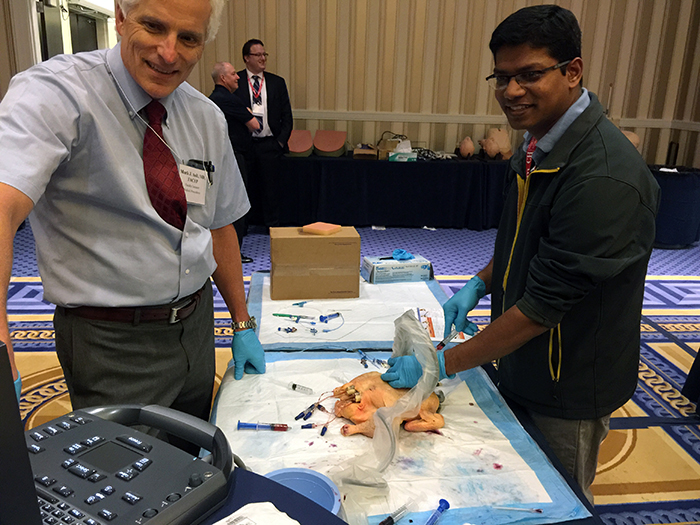
Dr. Ault, considered a pioneer in procedural medicine, often used chickens as teaching tools in his courses.
Over the past 30 years, the number of procedures performed by internists has steadily declined.1 Concordantly, the requirement to complete a minimum number of procedures during residency for board certification by the American Board of Internal Medicine was removed in 2007. As interest in performing procedures declined among internists and increased among other specialties, procedural medicine evolved into a profession all its own. Hospitalists have been at the forefront of this shift, developing medical procedure services (MPS) across the country.
It’s difficult to say exactly when MPS first came into existence, but Mark J. Ault, MD, who passed away earlier this year, co-founded Cedars-Sinai’s Outpatient Procedure Center in 1989. Dr. Ault is considered a true pioneer in the field. Hospitalist procedure services started springing up in teaching hospitals in the early 2000s,2 just a few years after the term “hospitalist” was coined in a 1996 New England Journal of Medicine article.3
MPS include physicians and advanced practice professionals who’ve chosen to dedicate a significant amount of their clinical time to performing invasive procedures such as paracentesis, vascular access, and thoracentesis. In teaching hospitals, proceduralists further play an important role in training students and residents. The structure of MPS varies by institution, but its benefits are enjoyed by hospitals, trainees, and patients alike. MPS streamlines hospital care by allowing for more timely bedside procedures and improved diagnostic accuracy. Trainees enjoy direct supervision and higher rates of learner satisfaction that surpass the “see one, do one, teach one” approach of the past.2,4 Patients enjoy safer procedures and more accurate diagnosis and treatment.
SHM and procedural medicine
SHM supports procedural training for hospitalists in myriad ways.5 In 2019, for example, the Society published a position statement with evidenced-based recommendations on the use of point-of-care ultrasound (POCUS) for diagnosis and bedside procedures in hospital medicine.6 SHM also partners with other organizations like the American College of Chest Physicians to offer POCUS courses, both live and online. And SHM offers a POCUS Certificate of Completion.7
Certification doesn’t instantly equate to competency, but it’s a step in the right direction. To earn SHM’s certification, participants must:
- Attend the Ultrasonography: Essentials in Critical Care course at the American College of Chest Physicians headquarters
- Complete one of the online learning modules
- Attend one of several approved regional courses
- Complete an online image portfolio
- Pass a comprehensive skill and knowledge assessment

Dr. Williams
Jason Williams, MD, an associate professor of medicine at Emory University School of Medicine in Atlanta, led the popular Ultrasound-guided Procedures course at SHM Converge 2022 in Nashville, Tenn., in April, and led procedure services at the University of California, Los Angeles, and the Atlanta Veterans Affairs Medical Center.
He says once you’ve completed 500-1,000 ultrasound-guided procedures you see the rare complications more frequently, so you’re better equipped to help other learners troubleshoot.
“The SHM POCUS certification is valuable for learners who don’t have someone to mentor them at their own hospital,” he said. “Workshops are good for skill foundation, but you’ve got to go back to your own patient population to practice. The value of the certification is the portfolio part. You need mentors to review your images so you can improve your image quality since POCUS diagnostic and procedural accuracy depend on it. That’s where the image portfolio comes in. An expert faculty reviewer provides prompt feedback about how to improve image acquisition. They let you know which images are adequate for clinical decision making, and which require optimization.”
SHM members can also join the POCUS Special Interest Group (SIG). This SIG, chaired by Benji Mathews, MD, FACP, chief of hospital medicine, Regions Hospital at HealthPartners and the University of Minnesota Medical School in St. Paul, Minn., and Gordon Johnson, MD, FACP, medical director of POCUS at Legacy Emanuel Medical Center in Portland, Ore., is a community of POCUS enthusiasts who are making positive contributions to hospital medicine and health care in general.
POCUS in diagnosis
POCUS also has applications for bedside diagnosis. As POCUS has become more accessible, more and more hospitalists are integrating its use into daily practice. POCUS is a valuable tool for the assessment of central venous pressure (CVP), identification of pleural and pericardial effusions, and/or alveolar filling processes. It also may be useful for evaluating response to therapy (e.g., serial volume-status exams while diuresing patients in acute decompensated heart failure (ADHF)).
Data demonstrating the efficacy of POCUS may surprise many readers. For example, POCUS was found to be six times more sensitive at detecting elevated CVP than physical exam8 and first-year medical students were found to be better at diagnosing ADHF with POCUS than cardiology fellows using the standard physical exam alone. 9
Dr. Williams said, “I really see POCUS augmenting the physical exam to allow us to miss fewer common diagnoses. I used to think that a great diagnostician discovered those rare zebra cases a few times a year. But now I realize that great diagnosticians are the ones who don’t miss the common things. They don’t confuse ADHF with pneumonia or chronic obstructive lung disease. With POCUS, we’re able to sort out normal from high CVP, and wet from dry lungs at the bedside in a matter of minutes.”
The future of procedural medicine

Dr. Liu
So where should hospitalists take procedural medicine from here? Gigi Liu, MD, MSc, an assistant professor of medicine and director of POCUS Education at the Osler internal medicine residency program at Johns Hopkins University School of Medicine in Baltimore, offered practical insight in this regard. “The future of procedural medicine is not in academic centers—it’s in rural settings,” she said.
“Many physicians are interested in diagnostic POCUS—national courses are selling out like crazy!—but that comes with upfront costs that hospitals might not be willing or able to cover,” she said. “The way to make diagnostic POCUS a reality is by starting with an MPS. Billing for procedures is straightforward, whereas it’s not for diagnostic POCUS. And MPS can cut the length of stay, offload interventional radiology, open hospital beds, and improve patient safety and satisfaction. MPS is thus attractive to hospital administrators and brings in revenue to cover initial sunk costs. Then, you use that money to push for the supplies and training needed to institute diagnostic POCUS.”
Procedural medicine is here to stay, and its beneficial impact is already evident. Trailblazers like Dr. Ault empowered hospitalists interested in procedures to truly come into their own. How might MPS and diagnostic POCUS help you and your patients? It’s never too late to find out.
Samantha C. Shapiro, MD, is a board-certified internist, rheumatologist, and affiliate faculty member of the Dell Medical School at the University of Texas at Austin. She received her training in internal medicine and rheumatology at Johns Hopkins University, Baltimore.
Celebrating the Memory of Dr. Mark Ault
Mark J. Ault, MD (June 10, 1952-February 14, 2021)

Dr. Ault
Dr. Ault was a pioneer of procedural medicine and a physician at Cedars-Sinai in Los Angeles for more than 40 years. He co-founded Cedars-Sinai’s Outpatient Procedure Center in 1989 and served as its director until his passing. In 2019, he was awarded Cedars’ inaugural Master Clinician Award for “outstanding leadership in advancing Cedars-Sinai’s mission and providing technically outstanding, patient-centered care.”
Dr. Ault earned his medical degree from the Icahn School of Medicine at Mount Sinai in New York and completed his residency at Cedars-Sinai. He was board certified in internal medicine, critical care medicine, and emergency medicine, and he was well published.
“As a person, Dr. Ault was a warm and gentle soul. He was so accomplished, but so down-to-earth and always open to learning new things,” said Nilam Soni, MD, MS, SFHM, FACP, professor of medicine at the Long School of Medicine at the University of Texas in San Antonio, Texas. “He was the senior person who helped develop SHM’s procedural pre-course, which still runs today. He set up a unique service at Cedars that’s still talked about around the country, and he was a mentor and inspiration for a lot of other internists. He showed us that you don’t have to be an interventionally trained person to do these procedures safely when you have US-guidance at your disposal. He really reinvigorated the procedural aspect of internal medicine.”

Dr. Soni
Dr. Soni is an internationally recognized leader in POCUS. In fact, he wrote the book on it; he’s the lead author of “Point-of-Care Ultrasound” (Elsevier, 2015) and has collaborated with myriad health care professionals to develop training curricula for different specialties.
Weijen Chang, MD, is a pediatric and adult hospitalist at Baystate Medical Center and Baystate Children’s Hospital in Springfield, Mass. where he is an associate professor of pediatrics at the University of Massachusetts Medical School Baystate, chief of pediatric hospital medicine, and vice-chair for clinical affairs at Baystate Children’s Hospital. He’s also the physician editor for The Hospitalist. Dr. Chang met Dr. Ault as a procedural pre-course faculty member.
“Dr. Ault approached teaching in a very non-judgmental manner,” he said. “He was all about getting it done, but getting it done in a way that was good for the learner as well as the patient.”

Dr. Chang
Dr. Chang shared details about the course itself, adding, “The whole course was really a family endeavor. The models for central line placement were these chickens that he, his wife, and his son would bring in from the supermarket. As you can imagine, transporting 20 raw chickens with tubes sticking out of them was a bit of a project. It was such a unique experience—we all felt like we were part of the Ault family for the day. They were so enthusiastic about procedural medicine and trying to improve the quality of training and care for patients, residents, and hospitalists.”
In Dr. Ault’s memory, Cedars-Sinai is raising funds to support specialized training and continuing education at the institution.
References
- Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: A resurvey of members of the American College of Physicians. Ann Intern Med. 2007;146(5):355-60. doi:10.7326/0003-4819-146-5-200703060-00007.
- Franco-Sadud R, et al. Hospitalist procedure services. SGIM Forum. 2016;39(5). Available online at https://www.sgim.org/File%20Library/SGIM/Resource%20Library/Forum/2016/SGIMMay2016_05r.pdf. Accessed June 28, 2022.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7)514-7. doi:10.1056/nejm199608153350713.
- Hayat MH, et al. Medical procedure services in internal medicine residencies in the US: a systematic review and meta-analysis. J Gen Intern Med. 2021;36(8):2400-07. doi:10.1007/s11606-020-06526-2
- Point-of-care ultrasound for hospitalists. SHM website. https://www.hospitalmedicine.org/clinical-topics/ultrasound/. Accessed June 28, 2022.
- Soni NJ, et al. Recommendations on the use of ultrasound guidance for adult lumbar puncture: a position statement of the Society of Hospital Medicine. J Hosp Med. 2019;14(10):591-601. doi:10.12788/jhm.3179
- POCUS Certificate of Completion. SHM website. Available at https://www.hospitalmedicine.org/clinical-topics/ultrasound/pocus-certificate-of-completion/. Accessed June 28, 2022.
- Brennan JM, et al. A comparison by medicine residents of physical examination versus hand-carried ultrasound for estimation of right atrial pressure. Am J Cardiol. 2007;99(11):1614-6 doi:10.1016/j.amjcard.2007.01.037.
- Kobal SL, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96(7):1002-6. doi:10.1016/j.amjcard.2005.05.060