In addition to all the fear and chaos it has wreaked, COVID-19 has changed the way we think about our health. Thanks to the psychological, and even the physical, impacts of protracted quarantines and shutdowns, many of us have come to realize that feeling healthy is more than the absence of disease. We feel our healthiest when experiencing positive emotions, when feeling calm and at peace, when connecting with others, and when taking in beauty with a sense of wonder.
So, isn’t it the right time for our health care system to start explicitly prescribing a dose of what we’re all finding to be true? Could clinicians shift the dominant paradigm on health just as dramatically as we are bringing vaccines to millions? Shouldn’t our patients expect more than pharmaceuticals from those who provide their health care?
A few of my colleagues and I are trying to do this now. Although I’m in awe when we dramatically change the course of diseases in the hospital with technological fixes, I also feel frustrated that my patients can leave the hospital believing that health is derived from pills and procedures. With the help of the Greater Good Science Center, my colleagues and I have started giving “old school” paper prescriptions to do things we all understand are good for us and for which there is sound scientific evidence.
Here are 10 prescriptions and the rationale for their use:
Take a few deep breaths. We all know a deep breath helps us relax. No surprise then that decades of research have demonstrated that by taking slow deep breaths, we calm the body and mind by activating the parasympathetic nervous system. When this happens, cortisol, heart rate, and blood pressure decrease. Taking deep breaths throughout the day can help keep us calmer and more balanced.
Call an old friend. Groundbreaking work by Julianna Holt-Lunstad1 suggests that social connection’s impact on mortality is on par with blood pressure, cholesterol, and obesity. The benefits likely come from the immediate activation of pro-social emotions and the long-term benefits of social support. This might be particularly helpful for our patients who are facing serious health challenges.
Give someone a hug. Hugging releases oxytocin2 which helps build social bonds and lowers the level of cortisol. When hugging, we also release endorphins which contribute to a sense of well-being and relaxation. But does anyone really need data to tell us hugs are good?
Help a friend in need. Helping others allows us to meet some important psychological needs3 such as developing our senses of agency and competence as we strengthen social relationships. When we act on our values by being good friends and helping those in need, we foster a sense of purpose that is foundational to a meaningful life. Research by Stephanie Brown4 suggests that those providing help may get more benefits than those receiving it. As hospitalists, it’s easy to lose contact with all the help we do. Consciously taking in all the good we do is a simple hack to bring more calm, connection, and meaning to our lives.
Write a thank-you note. Many studies over the last two decades have found that people who express gratitude are happier and less depressed. While one thank-you note is not the kind of gratitude practice that leads to lasting, positive, cognitive change, I tell my patients that their notes should be the beginning of a habit of counting their blessings in writing.5
Sing in the shower. Making music, and in particular singing, just makes us feel better. This happens through several mechanisms.6 We release endorphins when we sing; given this, it’s not surprising that singing reduces pain. Cortisol levels fall, leading to improved immune function. We make meaning as we embody the lyrics. I often add that people should join a choir, as singing surrounded by others greatly magnifies the benefits of singing. For my isolated older patients, I feel that encouraging them to join a choir might honestly be one of the best things I could do for their overall well-being.
Dance to your favorite song. We all know moving our bodies improves our health, but moving to music has additional benefits.7 The mood boost from dancing lasts much longer than exercise alone. And dancing often has social benefits. There’s even data suggesting dancing prevents cognitive impairment in the elderly.
Go for a walk in a beautiful place. We feel better being in nature, yet we underestimate the healing power of these experiences. Unfortunately, many of those I take care of have mobility issues and social circumstances that make this hard to do. I always recommend “awe walks”8 for those who are able. And for those who aren’t, I encourage finding ways to get to a place where nature can have its healing effects—even if it’s just the courtyard at the skilled nursing facility.
Forgive someone. Forgiveness doesn’t mean denying we were wronged; it means we let go of our anger and other unhealthy cognitive processes. Forgiveness requires hard work, but the benefits are profound: those who have learned to forgive live longer9 because there’s less stress and depression and better sleep and relationships.
Talk to yourself in a kinder voice. We’re often our own worst critics and when our health goes bad, we can cast an unhealthy amount of blame on ourselves. Self-compassion helps us heal ourselves rather than hurt ourselves. Talking to ourselves in a kinder voice is the key to this practice!10
As I make my rounds and prepare people for discharge, I write different happiness prescriptions to match what I believe to be the patient’s values and passions—all include the added direction to “Spread the Love”. I tell my patients at the end of the day, that there’s no better medicine than love.11 The more we love, the better and longer we live. I encourage them to keep this idea and love in their hearts. For the more curious, I recommend practicing a loving-kindness meditation; research suggests it can help us feel more love.12
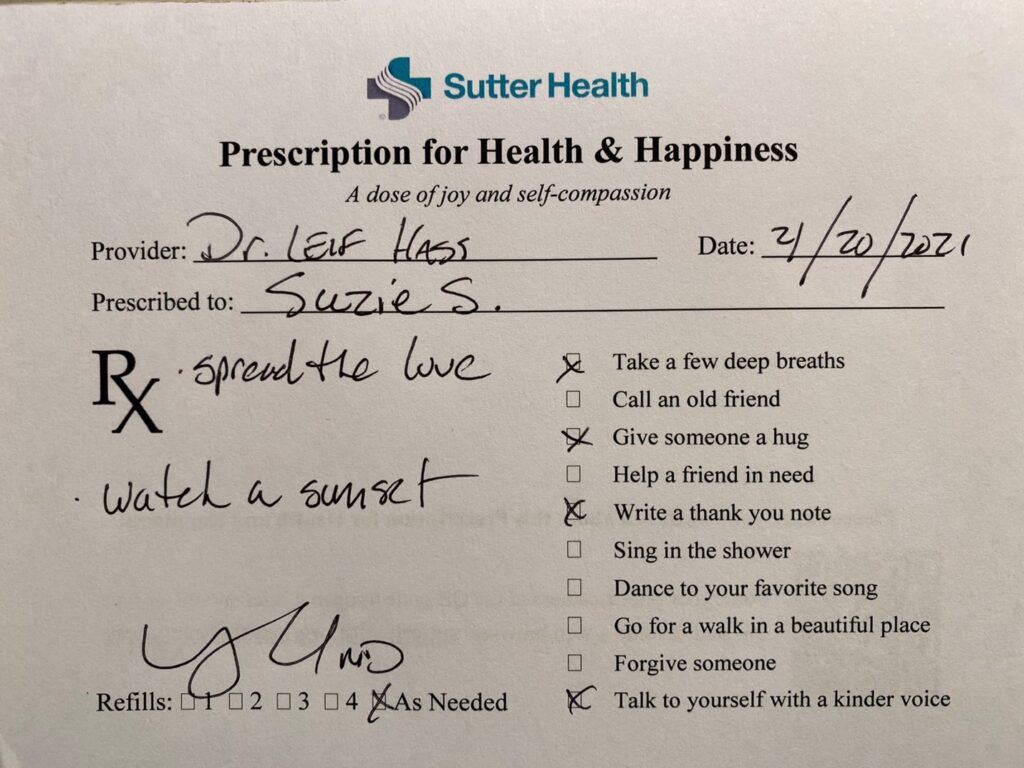
Prescriptions for health and happiness
Inevitably, these prescriptions are met with surprise, and often, joy. In 25 years of practicing medicine, I don’t recall any of my pharmaceutical prescriptions being met with such enthusiasm or being the topic of an Instagram post, as my happiness prescriptions have been known to be!
Sometimes, these prescriptions are met with tears. Ms. S—a tall, elegant, 69-year-old woman who’s battling cancer—was recently admitted to the hospital with a urinary tract infection and weakness. During my visits, her sadness permeated the room. Depression appeared to be her biggest challenge at that moment.
“Dr. Hass, I have lost my way,” she said, after describing to me her wavering faith. I handed her a prescription to “Join your church’s Zoom Bible study.”
Tears welled up and she said, “Bless you, I do need more than chemo to make it through. Ooh! Do I need this prescription!”
These prescriptions don’t just help patients. In our pilot study, 90% of doctors felt the prescription helped them connect with their patients and brought them joy personally. I find that talking about the ideas covered by these prescriptions has markedly improved my sense of well-being. Plus, it’s just darn fun to offer my patients the gift of love and joy!
The deprivations of the pandemic have led many of us to envision the selves we want to be—doctors and patients alike. These prescriptions can help us clarify this idea. And they are action plans that can offer ideas beyond what we originally might have considered. Research suggests when we act on a plan with intentionality, we change our cognitive architecture in ways that make the experiences felt more intensely. To add to this effect, I tell my patients to share the prescription and what they plan to do with family and friends, get others to join them, and post it on the fridge or social media.
This pandemic will lead to lasting social changes. Redefining our notion of health should be one of them. These happiness prescriptions explicitly state what we know to be true in our own lives, but so seldom say in the hospital: there are activities and habits of mind that have profound effects on health and well-being; such happiness-promoting activities can be as valuable to our health as many of the medicines we routinely prescribe. Hospitalists should be part of a medical culture that leads this paradigm shift. Prescription health and happiness should be a central part of what we do in hospital medicine.
If you’re interested in getting and using these prescriptions for yourself or your practice, email [email protected]. Feel free to reach out to me as well.
Dr. Hass is a hospitalist at Sutter East Bay Medical Group in Oakland, Calif., a member of the clinical faculty at the University of California, Berkeley-UC San Francisco joint medical program, and an adviser on health and health care at the Greater Good Science Center at UC Berkeley.
References
- Holt-Lunstad J, et al. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010 Jul 27;7(7):e1000316.
- McGlone F, Walker S. Four ways hugs are good for your health. Greater Good Magazine. 2021 June 22.
- Suttie J, Marsh J. 5 ways giving is good for you. Greater Good Magazine. 2010 Dec 13.
- Brown SL, et al. Providing social support may be more beneficial than receiving it: results from a prospective study of mortality. Psychol Sci. 2003;14(4):320-7.
- Brown J, Wong J. How gratitude changes you and your brain. Greater Good Magazine. 2017 Jun 6.
- Launay J, Pearce E. The new science of singing together. Greater Good Magazine. 2015 Dec 4.
- Predovan D, et al. Effects of dancing on cognition in healthy older adults: a systematic review. J Cogn Enhanc. 2019;3(2):161-167.
- Sturm VE, et al. Big smile, small self: awe walks promote prosocial positive emotions in older adults. Emotion. 2020. https://doi.org/10.1037/emo0000876
- Toussaint LL, et al. J Behav Med. 2012 Aug;35(4):375-86.
- Greater Good in Action. https://ggia.berkeley.edu/practice/self_compassion_break. Accessed February 28, 2022.
- Zeng X, et al. The effect of loving-kindness meditation on positive emotions: a meta-analytic review. Front Psychol. 2015; 6: 1693. Published online 2015 Nov 3.
- Loving-kindness meditation. Greater Good in Action. https://ggia.berkeley.edu/practice/loving_kindness_meditation. Accessed February 28, 2022.
