Clinical decision making
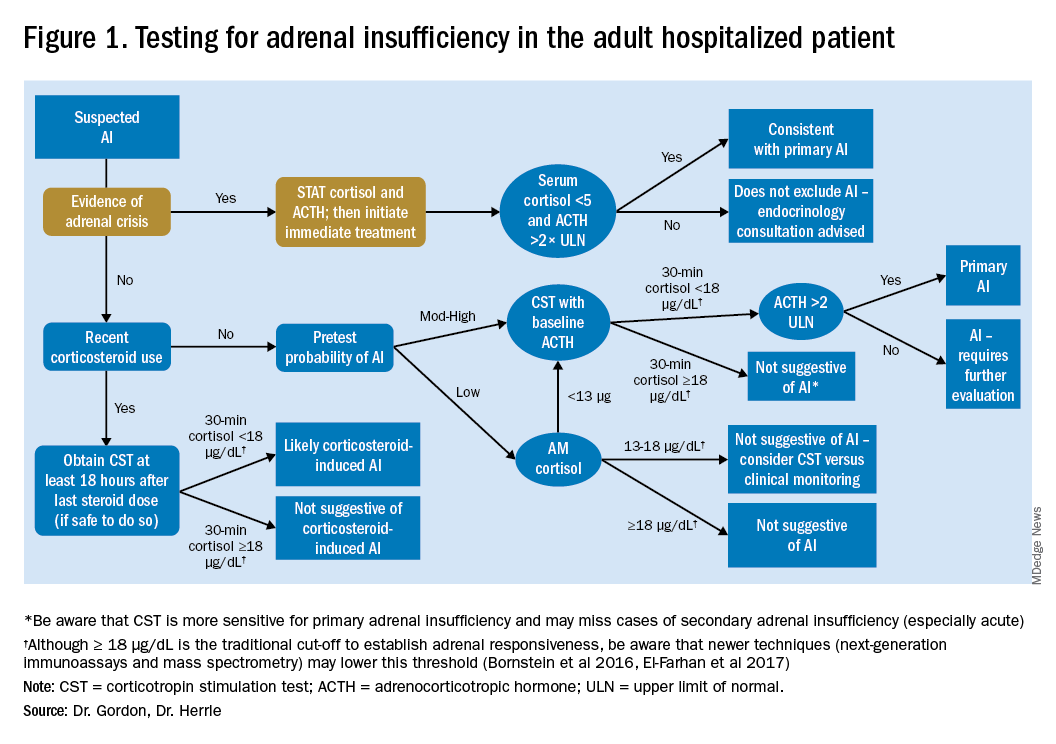
Diagnostic evaluation should be guided by the likelihood of the disease (i.e., the pretest probability) (Figure 1). Begin with a review of the patient’s signs and symptoms, medical and family history, and medications with special consideration for opioids, exogenous steroids, and immune checkpoint inhibitors (Table 1).
For patients with low pretest probability for AI, morning cortisol and ACTH is a reasonable first test (Figure 1). A cortisol value of 18 mcg/dL or greater does not support AI and no further testing is needed.2 Patients with morning cortisol of 13-18 mcg/dL could be followed clinically or could undergo further testing in the inpatient environment with CST, depending upon the clinical scenario.4 Patients with serum cortisol of <13 mcg/dL warrant CST.
For patients with moderate to high pretest probability for AI, we recommend initial testing with CST. While the results of high-dose CST are not necessarily impacted by time of day, if an a.m. cortisol has not yet been obtained and it is logistically feasible to do so, performing CST in the morning will provide the most useful data for clinical interpretation.
For patients presenting with possible adrenal crisis, it is essential not to delay treatment. In these patients, obtain a cortisol paired with ACTH and initiate treatment immediately. Further testing can be deferred until the time the patient is stable.2
Potential pitfalls
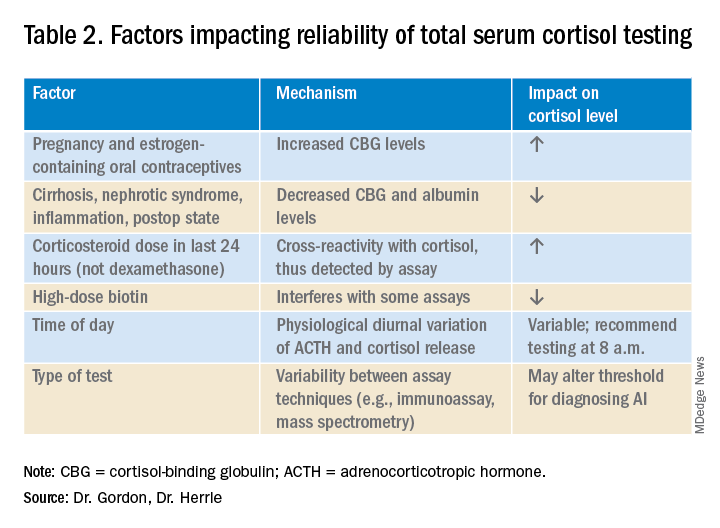
Interpreting cortisol requires awareness of multiple conditions that could directly impact the results.2,3 (Table 2).
Currently available assays measure “total cortisol,” most of which is protein bound (cortisol-binding globulin as well as albumin). Therefore, conditions that lower serum protein (e.g., nephrotic syndrome, liver disease, inflammation) will lower the measured cortisol. Conversely, conditions that increase serum protein (e.g., estrogen excess in pregnancy and oral contraceptive use) will increase the measured cortisol.2,3
It is also important to recognize that existing immunoassay testing techniques informed the established cut-off for exclusion of AI at 18 mcg/dL. With newer immunoassays and emerging liquid chromatography/tandem mass spectrometry, this cut-off may be lowered; thus the assay should be confirmed with the performing laboratory. There is emerging evidence that serum or plasma free cortisol and salivary cortisol testing for AI may be useful in certain cases, but these techniques are not yet widespread or included in clinical practice guidelines.2,3,7
Population focus: Patients on exogenous steroids
Exogenous corticosteroids suppress the HPA axis via negative inhibition of CRH and ACTH release, often resulting in low endogenous cortisol levels which may or may not reflect true loss of adrenal function. In addition, many corticosteroids will be detected by standard serum cortisol tests that rely on immunoassays. For this reason, cortisol measurement and CST should be done at least 18-24 hours after the last dose of exogenous steroids.
Although the focus has been on higher doses and longer courses of steroids (e.g., chronic use of ≥ 5 mg prednisone daily, or ≥ 20 mg prednisone daily for > 3 weeks), there is increasing evidence that lower doses, shorter courses, and alternate routes (e.g., inhaled, intra-articular) can result in biochemical and clinical evidence of AI.9 Thus, a thorough history and exam should be obtained to determine all recent corticosteroid exposure and cushingoid features.