“Taking care when prescribing medications for the elderly, guarding against the dangers of polypharmacy, and avoiding restraints in cases of delirium not only prevent costly overtreatment but can help maintain the patient’s level of function,” Dr. Parks says.
4 An interdisciplinary approach is most effective for geriatric patients.
Dr. Parks also advocates for team-based care, with hospitalists working collaboratively to bring multiple perspectives to treating the patient.
“The team not only works together to develop a treatment plan but leverages their diverse perspectives to align their treatment plan with the patient’s and family’s needs and individual goals for care,” she says. “This becomes increasingly important as geriatric patients approach the end of life.”
5 Guard against delirium.
Delirium is one of the most common occurrences among geriatric patients.
“While more and more frontline providers are familiar with delirium, most hospital units and the systems of care delivery are not designed to prevent delirium or treat it once it has developed,” Dr. Mattison says. “For instance, while we know the importance of proper sleep and ensuring patients are allowed uninterrupted sleep at night, we still frequently wake patients multiple times per night. Multiple clinical providers have different jobs to do during the night—the aide will wake the patient to check vital signs, the nurse will later wake the patient to dispense a necessary medication, the phlebotomist will wake the patient to draw blood.”
These practices, common in hospitals, are contributing to the prevalence of delirium among geriatric patients.
Dr. Parks warns that dementia patients are at an “especially high risk for delirium and must be observed more closely.
“Because of its transitory nature, delirium is easy for a physician to miss,” she adds. “In fact, another benefit of the team-based approach is that the more physicians [there are] who evaluate a geriatric patient, the greater the chances [are] that delirium will be caught.”
6 Beware the dangers of polypharmacy and medications that pose risks to older adults.
Polypharmacy in the elderly has been associated with significant negative consequences, including increases in healthcare costs, adverse events, and falls, and decreases in nutrition and overall functional status.3
According to Dr. Parks, polypharmacy is a major contributor to delirium; to avoid it, medication lists should be pared down when possible, and the Beers Criteria list should always be consulted when prescribing a new medication. Beyond lists, electronic medical records can provide interventions that can offer embedded medication decision support.
Dr. Mattison says her hospitalist team is fortunate, because the systems Beth Israel Deaconess has in place help improve medication safety for the elderly.
“[We] have a proprietary system that has allowed us to customize alerts and embed decision support,” she explains. “We have selected drug warnings drawn from lists of potentially inappropriate medications for elders [and] embedded decision support screens to guide ordering providers, making it easier to ensure the right drug in the right dose is ordered for the right patient at the right time.”
Hospital Elder Life Program (HELP) Interventions
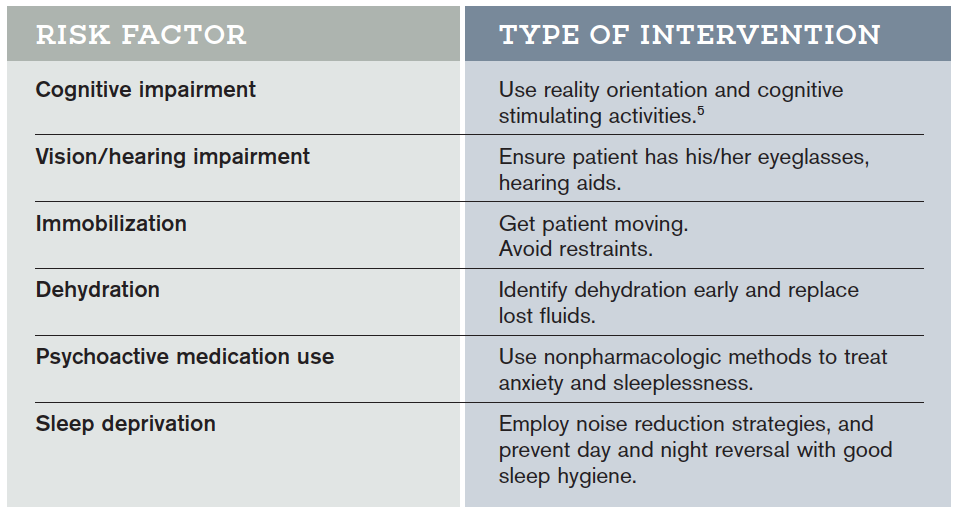
Hospital Elder Life Programs (HELP) are integrated units of care designed to prevent delirium by employing clinically proven interventions in the presence of specific delirium risk factors.5
7 Think in terms of syndromes, rather than independent causes.
“When an elderly patient presents with conditions such as post-operative delirium, incontinence, or an increased risk for falls, there are usually multiple contributing factors rather than a unique cause,” Dr. McCormick says. “Syndromatic thinking enables you to identify multiple potential factors and treat all of them, hoping that in aggregate the treatments will improve the patient’s condition.”

Is it common for geriatricians not to make rounds on their elderly hospitalized patients and to leave their care to the hospitalist? Wouldn’t this create panic in the patient to be cared for face-to-face by a doctor who is unknown to the patient and whom the hospitalist does not know?