The average daily census (ADC) is a tool that has been used in healthcare to “effectively manage patient flow, allocate resources, and ensure high-quality care.” It has become a central part of staffing decisions, which makes it a major component of how we hospitalists start our day or night shifts. However, is the midnight ADC the best time to measure? Drs. Logan Pierce, Timothy Judson, and Michelle Mourad teamed up to write an analysis of ADC as it varies throughout the day, in the Journal of Hospital Medicine Brief Report, “Finding the time: Hourly variation in average daily census on a hospital medicine service.” This article was the subject of February 2024’s #JHMChat. In addition to Drs. Pierce and Judson, we were joined by guest experts Dr. Rebecca Jaffe, Dr. Dimitriy Levin, Dr. Marisha Burden, and Dr. Alan Kubey.
The conversation started with participants’ experiences with ADC use at their institutions. A universal sentiment was that a higher census makes the day increasingly more challenging. Features like a census cap, swing shift clinicians, and staffing adjustments during surges were key to managing census and hospitalist well-being.
Dr. Burden emphasized the importance of staffing buffers to absorb high total census, and how short-staffed hospitals suffer increased costs in the long run (locums, length of stay, burnout). Dr. Judson pointed out how, to avoid compromising the quality of care in times of high census, hospitalists may defer important but time-consuming tasks like discharge planning.
In addition to day-to-day staffing, multiple participants pointed out how ADC over time determines how many inpatient teams will be funded.
Dr. Levin discussed an alternative to ADC, focusing on census related to work.
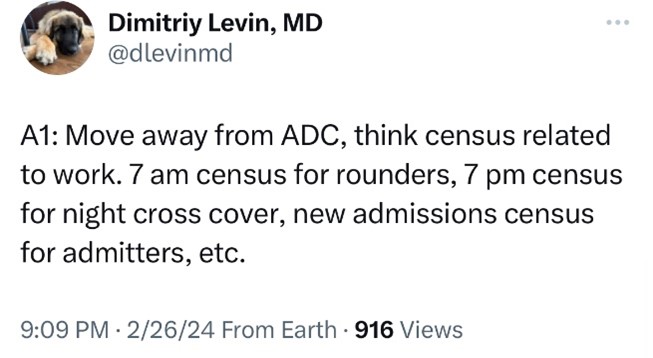
In the Brief Report, ADC generally peaked around 11:00 AM. The variety in systems was again present here, as people discussed the moving target of “discharge by X time” policies and how the census gets monitored throughout the day. Some hospitalists are made aware of these fluctuations, but many are not informed. The benefits of interdisciplinary rounds, whether in the morning or afternoon (or a huddle to discuss the following day), are also readily apparent. Dr. Burden, riding a proverbial surfboard along the tidal waves of data, discusses her #EvidenceBasedWorkDesign in optimizing staffing strategy with real-time data based on these fluctuations. Dr. Alan Kubey chimed in, elaborating on her work on the “workload score” taking into account admissions, discharges, transfers, outside hospital inbound, and more. A single source of view-only data for team census and flow can help ensure transparency.
When is an admission most disruptive? Pre-/intra-rounds or afternoon? Can swing positions be adjusted for that? We look to our surgical and nursing colleagues who utilize dynamic staffing based on cases scheduled or patients on the floor. Does a separate admitting hospitalist alleviate this issue? Dr. Astik talks about a recent adaptation in which a triage nurse “holds the admissions pager, fields calls, and tracks admits” to allow “admitters to see patients with less pages.”
Looking to the future, Dr. Judson suggested assistance by artificial intelligence or machine learning to help optimize dynamic staffing. Meanwhile, in the present, Dr. Rebecca Berger and other hospitalists at other institutions are only seeing 2023 data now to try and adjust staffing…
Dr. Burden, with my personal favorite Tweet of the evening, pointed out that it is often thought that “short-staffing is cheaper… (i.e. running higher patient to clinician ratios) but insufficient staffing affects throughput and costs directly in addition to demoralizing the workforce.” She drove it home by citing the paper “Mixing It Up: Operational Impact of Hospitalist Caseload and Case-mix” by Kamalahmadi et al.
The final topic of the #JHMChat discussed partnering with administrators to address these issues. Dr. Jaffe kicked open my mental doors to start, as I half-jokingly referenced the outdated metric of “Discharge by X time” but she twisted it on its ear by proposing it as a goal and measurement used to shape and justify staffing, rather than as a metric.
Dr. Judson’s institution has a backup pool of providers who can be called upon to come in and help when admissions surge. Dr. Levin emphasized the importance of funding a data team to generate daily reports and rapid feedback on census and staffing.
Average daily census, as it shapes the daily lives of hospitalists and their workloads, remains an important topic even as its measurement and timing evolve to better suit staffing needs. We can continue to learn from other hospitalists and bring innovations (including moving away from the ADC as the basis for staffing!) to our own institutions in order to provide better care for our patients.
Please search #JHMChat to read these and more insightful posts, and we will see you at an upcoming #JHMChat! You can also read the full article in the Journal of Hospital Medicine.
Dr. Thomas is a hospitalist with Buffalo Medical Group and clinical instructor with the community-based Catholic Health Internal Medicine Residency in Buffalo, N.Y. He is also a deputy editor, digital media for the Journal of Hospital Medicine.