Case
A 77-year-old woman with malnutrition, who is undergoing chemotherapy for small cell lung cancer, is being treated with intravenous ceftriaxone and vancomycin through a peripherally inserted central catheter for vertebral osteomyelitis. After initial improvement on antibiotics, she develops a new fever with an increased white blood cell count of 3,400 per microliter. She is ill-appearing and septic with no overt source. Blood cultures are collected. A beta-D-glucan is 102 pg/mL.
 What is beta-D-glucan?
What is beta-D-glucan?
Beta-D-glucan is a polysaccharide found in the cell wall of vegetation such as barley and oats, and in the cell wall of bacteria, fungi, yeasts, and algae. The type of bonds between the glucose monomers differs between organisms. Beta-D-glucan in bacteria and algae are linear structures made of glucose monomers linked via B-(1->3) bonds. In yeast and mushrooms, the glucose monomers are linked via B-(1->3) and B-(1->6) bonds, creating a branched molecule. Commercial assays detect the common B-(1->3) component using the innate immune system of horseshoe crabs.1
Beta-D-glucan is commonly used as adjunct evidence to diagnose invasive fungal infections. In addition to immunodeficient diseases such as human immunodeficiency virus and hematological malignancies, the increase in immunosuppressive therapy in the medical field has increased opportunities for invasive fungal infections. Invasive fungal infections have attributable mortality of 30-40% in the U.S.1 Blood cultures are only positive in 50% of cases of invasive candidiasis and <10% of invasive aspergillosis.2 As a result, serum beta-D-glucan has been more frequently used to support clinical suspicion for fungal infections.
How to interpret beta-D-glucan

Nhi N. Vu-Ticar, MD
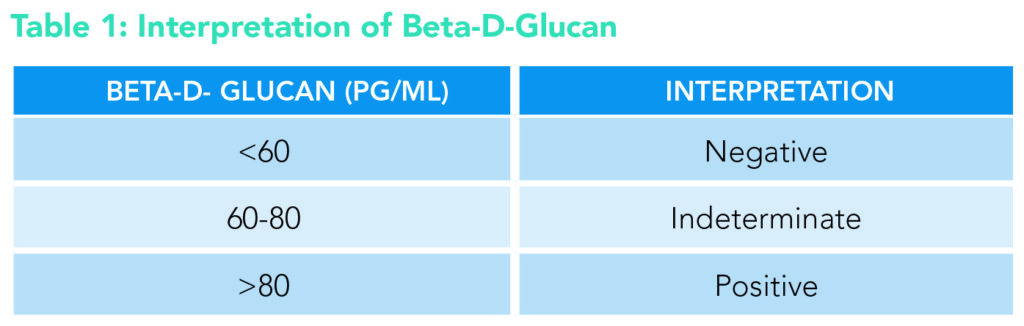
There are different beta-D-glucan assays used, with different cutoff points for optimal sensitivity and specificity depending on the assay. The three most commonly used assays are Fungitell (Associates of Cape Cod, Inc., Mass., U.S.), Fungitec-G test (Seikagaku Biobusiness, Tokyo, Japan), and Wako (Wako Pure Chemical Industries, Osaka, Japan). Fungitell is the U.S. Food and Drug Administration-approved test to be used in the U.S. and is the focus of this paper. Although testing for the same substrate, the assays use different reagents that can affect the optimal cut-off points. In general, these assays detect beta-D-glucan in the range of 0 to >7000 pg/mL. Many clinical studies have been performed to analyze the optimal cut-off points for these assays. Per a 2015 meta-analysis that included 28 different studies on the three mentioned assays, the cut-offs varied, but 60-80 pg/mL was determined to be the most reliable range for sensitivity and specificity for Fungitell assays.3 Per Fungitell’s manufacturer manual (Table 1), <60 pg/mL denotes a negative result, 60-79 pg/mL is indeterminate, and ≥ 80 pg/mL is positive.4

Adam J. Gray, MD
It is important to keep in mind that the sensitivities and specificities can differ among different species of organisms. According to a 2011 meta-analysis published in Clinical Infectious Diseases,1 beta-D-glucan typically has a sensitivity of 77% and specificity of 85% among Aspergillus infections compared to 81% and 60% respectively amongst Candida species. The sensitivity and specificity are increased in detecting Aspergillus infections when both beta-D-glucan and galactomannan are used together. Beta-D-glucan assays also have a strong negative predictive value and can be used to rule out invasive fungal infection (IFI) when suspicions are low. For a cut-off of 80 pg/mL, the assay has a positive predictive value of 89% and a negative predictive value of 73%.2 Although beta-D-glucan has high positive predictive value in Candida, Fusarium, and Aspergillus, the cut-offs are more precise for Candida.
When should beta-D-glucan be used? Beta-D-glucan can be used to help identify infections with Aspergillus, Candida, Pneumocystis jirovecii, or Fusarium. For invasive fungal infections, it is important to use clinical judgment and criteria developed by the European Organization for Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG) as the main tools for diagnosis. The criteria provide a more standardized approach in suspected invasive fungal infections. The criteria include patient factors such as neutropenia, use of steroids, and existing immunodeficiency, in addition to laboratory data such as culture and biopsy results. When clinical suspicion is moderate to high, beta-D-glucan and galactomannan can be used as an adjunct to support the diagnosis. It is particularly helpful and more sensitive than blood cultures in deep-seated candidiasis, as blood cultures are often negative.3 Another advantage of using beta-D-glucan is quick turnaround time, as it can take as little as one hour for the results.5 Beta-D-glucan can also be considered for surveillance in high-risk populations such as hematologic malignancy undergoing chemotherapy for earlier detection of invasive fungal infection.6
When should beta-D-glucan not be used? Beta-D-glucan is not found in all fungal species and cannot be used to identify infections by Cryptococcus, Blastomyces (yeast form), or Zygomycetes such as Absidia, Mucor, or Rhizopus since these species either do not produce beta-D-glucan or produce low levels that might lead to false negatives.
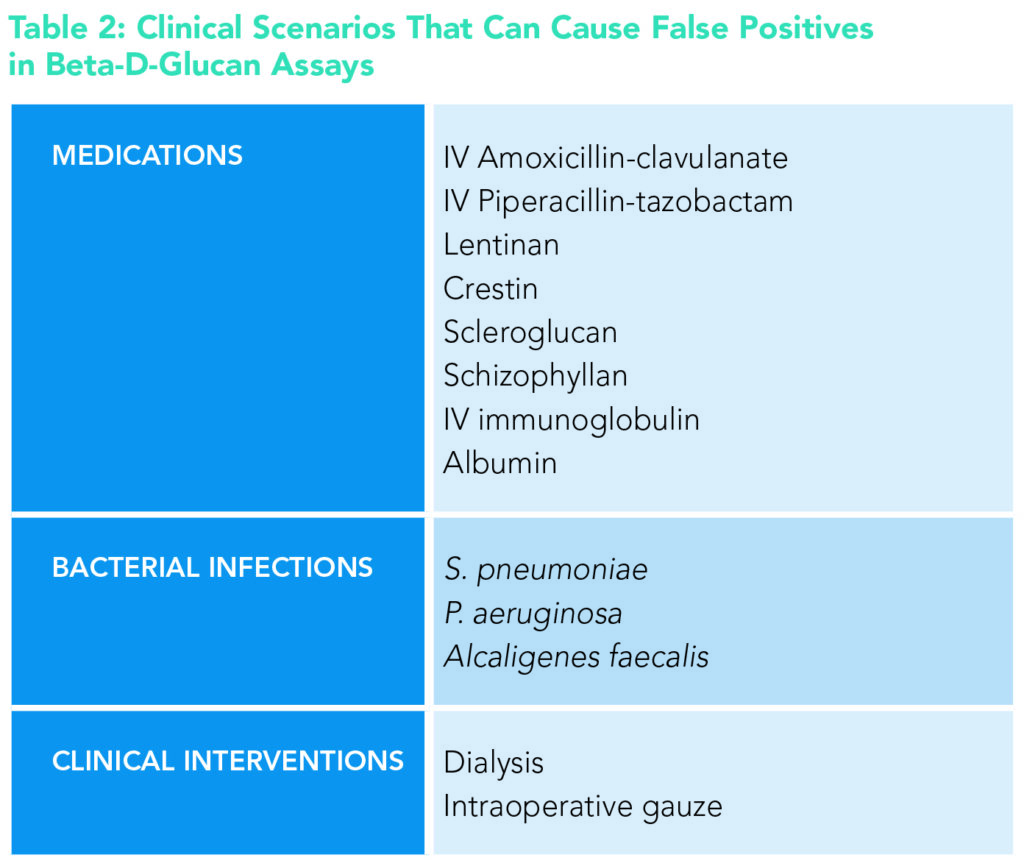
Clinicians should also be wary of scenarios that might lead to false-positive results. Certain medications can falsely elevate beta-D-glucan levels, including intravenous amoxicillin-clavulanate and piperacillin-tazobactam. Infections by certain bacterial organisms can also lead to false positives including S. pneumoniae and P. aeruginosa, both of which also produce beta-D-glucan. Another clinical scenario to be aware of is dialysis patients because beta-D-glucan is commonly tested in critically ill patients susceptible to invasive fungal infections. The cellulose filters used in dialysis release beta-D-glucan substrates that can lead to false positives. Table 2 lists some common situations that can lead to false-positive beta-D-glucan results.
 Application to the case
Application to the case
In the case presented, there is clinical suspicion for fungal infection given the patient’s immunodeficiency and worsening clinical condition on broad-spectrum antibiotics. Given the moderate pretest probability and the high beta-D-glucan, it would be appropriate to start antifungal therapy empirically while awaiting further diagnostic evaluation.
The patient was started on empiric micafungin. Two days later, blood cultures grew Candida albicans and the patient was diagnosed with catheter-associated Candidemia. Beta-D-glucan in this setting aided the decision to initiate earlier treatment of invasive fungal infection.
Bottom line
Beta-D-glucan should be used as an adjunct to support clinical judgment, in combination with EORTC/MSG criteria and other diagnostic tests (i.e. blood cultures, biopsies), when there is suspicion of invasive fungal infection.
Key Points
- A beta-D-glucan of >80pg/mL has a sensitivity of 0.83 and specificity of 0.84 for invasive fungal infection.
- Beta-D-glucan should be used in conjunction with clinical judgment, EORTC/MSG criteria, and other clinical tests including biopsies and fluid cultures.
- False-positive results are common including in dialysis patients, with certain medications such as piperacillin-tazobactam, and in some bacterial infections including S. pneumoniae and P. aeruginosa.
Quiz: Testing your knowledge
A 58-year-old woman with chronic obstructive lung disease and bronchiectasis presented with fever, cough, and dyspnea. She was found to have Pseudomonas aeruginosa bacteremia due to pneumonia. She was empirically treated with intravenous piperacillin-tazobactam.
During the evening of hospital day two, she had a temperature of 101.2 degrees Fahrenheit. The night provider ordered repeat blood cultures and a beta-D-glucan. Cultures are pending and beta-D-glucan was 64 pg/mL. The following morning, she reports overall feeling much better than admission with improved cough, dyspnea, and malaise.
What is the most appropriate next step in treatment?
A. Add fluconazole
B. Add micafungin
C. Add vancomycin
D. Continue piperacillin-tazobactam
The correct answer is D. Beta-D-glucan returned in the indeterminate range. This patient had a clear alternative etiology of symptoms given the Pseudomonas pneumonia and clinical suspicion for a secondary invasive fungal infection is low. This patient also has two alternative potential causes of elevated beta-D-glucan (pseudomonas infection, piperacillin-tazobactam). Given her overall clinical improvement on appropriate antibiotic therapy, it would be appropriate to continue her piperacillin-tazobactam.
Dr. Vu-Ticar is a hospitalist at the University of Kentucky, Lexington. Dr. Gray is a hospitalist at the University of Kentucky and the Lexington Veterans Affairs Medical Center.
Additional Reading
- Revised EORTC/MSG criteria: Donnelly JP, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium, Clin Infect Dis.2020;71(6):1367-1376. doi: 10.1093/cid/ciz1008. PMID: 31802125; PMCID: PMC7486838.
- Updates on new molecular tests for invasive fungal infections: Sanguinetti M, et al. Diagnosis and treatment of invasive fungal infections: looking ahead. J Antimicrob Chemother. 2019;74(Suppl 2):ii27-ii37. doi: 10.1093/jac/dkz041. PMID: 31222314.
- Epidemiology on invasive fungal infections in the United States: Webb BJ, et al. Epidemiology and clinical features of invasive fungal infection in a US health care network. Open Forum Infect Dis. 2018 Jul 31;5(8):ofy187. doi: 10.1093/ofid/ofy187.
References
- Karageorgopoulos DE, et al. B-D-glucan assay for the diagnosis of invasive fungal infections: a meta-analysis. Clin Infect Dis. 2011;52(6):750-770. doi:10.1093/cid/ciq206.
- Ostrosky-Zeichner L, et al. Multicenter clinical evaluation of the (1->3) beta-D-glucan assay as an aid to diagnosis of fungal infections in humans. Clin Infect Dis. 2005;41(5):654-659. doi:10.1086/432470.
- He S, et al. A systematic review and meta-analysis of diagnostic accuracy of serum 1,3-β-d-glucan for invasive fungal infection: Focus on cutoff levels. J Microbiol Immunol Infect. 2015;48(4):351-361. doi:10.1016/j.jmii.2014.06.009.
- About Fungitell. Fungitell website. Available at: https://www.fungitell.com/. Accessed July 1, 2022.
- Nguyen MH, et al. Performance of Candida real-time polymerase chain reaction, β-D-glucan assay, and blood cultures in the diagnosis of invasive candidiasis. Clin Infect Dis. 2012; 54(9):1240-8. doi: 10.1093/cid/cis200. Epub 2012 Mar 19. PMID: 22431804.
- Hammarström H, et al. How to interpret serum levels of beta-D-glucan for the diagnosis of invasive fungal infections in adult high-risk hematology patients: optimal cut-off levels and confounding factors. Eur J Clin Microbiol Infect Dis. 2015;34(5):917-925. doi:10.1007/s10096-014-2302-9.
Thank you for this excellent article. I work at a geriatric hospital in Japan, where invasive fungal infections are relatively frequent. I will share this article with my Japanese residents after I find the cut-offs for the test used locally.