Case
A 76-year-old man is diagnosed with non-valvular atrial fibrillation. His comorbid conditions are hypertension, diabetes complicated by neuropathy, and chronic kidney disease stage 3. His current medications include metformin, lisinopril, gabapentin, and aspirin. His most recent laboratories showed a creatinine 1.8, creatinine clearance (CrCl) 35 mL/min, hemoglobin 11g/dL, and international normalized ratio 1.0. His congestive heart failure, hypertension, age, diabetes, stroke, vascular disease, and sex (CHADSVASc) score is 4. Which medication should we use to prevent stroke in this patient?
Brief overview of the issue
Chronic kidney disease (CKD) affects approximately 15% of adults worldwide. This disease co-exists with other major cardiovascular diseases such as atrial fibrillation (AF). The prevalence of AF in CKD ranges between 12% and 18% in different studies and increases further with decreasing CrCl.1
Current guidelines recommend anticoagulation to reduce thromboembolic events in patients with AF if the CHADSVASc score is >2 for men and >3 for women. Warfarin is therapeutically satisfactory, but it is the narrow therapeutic window, complex drug-interaction profile, and need for frequent laboratory monitoring which makes it cumbersome for many patients.
Direct oral anticoagulants (DOACs) have emerged as a promising option because of more reliable anticoagulation activity at fixed dose and fewer drug-drug interactions (DDIs).2 Several well conducted, randomized, controlled trials (RCTs) have established DOACs as noninferior or superior to warfarin. However, the use of DOACs in CKD patients with AF remains controversial.
Review of available data
Several DOACs have been approved for the prevention of thromboembolic events in atrial fibrillation including apixaban, edoxaban, rivaroxaban (Xa inhibitors), and dabigatran (a thrombin inhibitor). Regardless of the mechanism of action, DOACs have been shown to be superior to warfarin for thromboembolic prevention and safer in terms of bleeding in patients with AF. However, this evidence is hard to extrapolate in patients with CKD.
DOACs have varying degrees of renal clearance and patients with advanced renal impairment (CrCl <30 mL/min) were excluded from most major trials. Specifically, the trials ROCKET AF, RE-LY, and ENGAGE AF-TIMI 48 excluded patients with a CrCl <30 mL/min. The ARISTOTLE trial excluded patients whose CrCl was <25 mL/min, and only 269 patients with CrCl 25-30mL/min were included.3
Considering all available data in patients with mild to moderate CKD, warfarin and DOACs have shown similar efficacy. In terms of safety profile, DOACs are noninferior or even superior to warfarin. Therefore, the Food and Drug Administration (FDA) has approved apixaban, rivaroxaban, dabigatran, and edoxaban in patients with CKD stages 1-3. Apixaban and rivaroxaban are the two DOACs that have been used the most in patients with advanced CKD (CrCl of <30 mL/min). Also, these are the only two DOACs with FDA approval for patients undergoing hemodialysis.
It is important to note that the FDA approval for these medications in advanced CKD was a result of small pharmacokinetics studies. Multiple authors have conducted retrospective studies with DOACs in advanced renal disease, but the results are inconsistent.4
Siontis et al studied a total of 26,111 patients with end-stage renal disease and AF, 2,351 of whom were on apixaban. The authors reported a decreased risk of bleeding in patients taking apixaban compared to warfarin with an equal risk of stroke, systemic embolization, and death. There was increased efficacy of apixaban 5 mg twice daily over warfarin in terms of stroke prevention and mortality, but not of the 2.5 mg dose.5
Mavrakanas et al showed that apixaban 5 mg twice daily in dialysis patients resulted in supratherapeutic levels, while a 2.5 mg dose did not.2
Shin et al retrospectively evaluated 20,727 patients with AF and CKD and found DOAC efficacy for stroke prevention was equal to that of warfarin, but there was a 23% higher risk of bleeding in patients taking DOACs with a CrCl <60 mL/min. However, only 4% of this patient cohort had CrCl <30 mL/min.6
Lastly, a recent systematic review, including 10 observational studies (three studies including patients with CrCl <25 mL/min), found no difference for stroke prevention in dialysis patients between the DOACs (apixaban, rivaroxaban, dabigatran) and warfarin. Rivaroxaban and dabigatran were associated with an increased major bleeding risk as compared to warfarin, but this was not seen with apixaban.7
Based on this study, the FDA recommended apixaban 5 mg in patients with dialysis. Further, they recommended that the 2.5 mg dose should be used only if the patient meets two of three characteristics, namely, Cr >1.5 mg/dL (133 mmol/L), age >80 years, or bodyweight <60 kg.5
Given the sparse evidence in CKD, it is safer to use warfarin in individuals with CKD stage 4-5 and AF as the recommendations for DOACS are inconsistent between societies.1-3 (Table 1).
Application of the data to our case
Our patient with a newly diagnosed AF and a CHADSVASc score of 4 will benefit from anticoagulation. Because his CrCl is >30 mL/min, DOACs can be used safely. Therefore, we can use either of the four available DOACs in our patient.
Bottom line
Literature suggests that DOACs are safe in patients with renal disease and CrCl >30. In this population, DOACs are not inferior when compared with warfarin both in terms of efficacy and safety.
Key Points
- DOACs are safe in patients with CKD and CrCl >30mL/min
- In patients with CrCl <30mL/min, data on DOACs are very limited; therefore, warfarin should be considered as first-line
- Apixaban seems to have the best side-effect and safety profiles in most studies
Quiz: Use of DOACs in patients with CKD
A 36-year-old man with a history of heart failure with reduced ejection fraction secondary to non-ischemic cardiomyopathy comes to the ED with a two-day history of diarrhea and palpitations. An ECG shows atrial fibrillation with a heart rate of 180. Basic laboratories showed Cr 2.2 CrCl 59, Na 157, and K 3.9. The patient received intravenous fluids and intravenous metoprolol leading to a controlled heart rate. The patient asks you what medication is the best option to reduce his stroke risk.
- Apixaban
- Warfarin
- Rivaroxaban
- None of the above
Correct option: 4. Patient’s CHADSVASc score is 1 (heart failure) therefore his stroke risk is low, and the experts recommend no anticoagulation in this group of patients.
A 77-year-old female with a history of hypertension, diabetes, gout, CKD stage 3, and atrial fibrillation comes to your clinic. She is worried about her atrial fibrillation and wants to know how she can decrease the risk of developing a stroke. Her medications include amlodipine, metformin, allopurinol, and amiodarone. Which of the following anticoagulants should we recommend in this patient?
- Apixaban
- Dalteparin
- Unfractionated heparin
- Warfarin
Correct option: 1. Apixaban will be the most appropriate option for this patient. Warfarin can also be used in CKD stage 3 but given that the patient is taking two drugs (amiodarone and allopurinol) that inhibit the metabolism of warfarin she is at a higher risk of bleeding, making apixaban the safest option in this case.
A 72-year-old man with a history of heart failure with reduced ejection fraction secondary to ischemic heart disease, diabetes, hypertension, and CKD comes to the ED complaining of new-onset palpitations. An ECG is obtained, and it shows atrial fibrillation. His current regimen includes metformin, lisinopril, and carvedilol. Laboratories show Cr 1.9, CrCl 20, hemoglobin 11g/dL. Which of the following drugs is the best next step?
- Apixaban
- Dabigatran
- Rivaroxaban
- Warfarin
Correct option: 4. In patients with CrCl <30, data supporting the safety and effectiveness of DOACs is very limited; hence warfarin would be the best choice for this patient.
A 69-year-old man with a history of coronary artery disease, ischemic cardiomyopathy, CKD, hypertension, and diabetes is diagnosed with atrial fibrillation. His most recent renal function panel showed a Cr 2.0, CrCl 24mL/min. Which of the following drugs will be the best option for anticoagulation?
- Apixaban
- Edoxaban
- Rivaroxaban
- Warfarin
Correct option: 4. There is not sufficient evidence supporting DOACs in patients with CrCl <30. Guidelines in this patient population are inconsistent. Therefore, until an RCT is performed to study the safety of DOACs in this population, warfarin will be the safest choice.
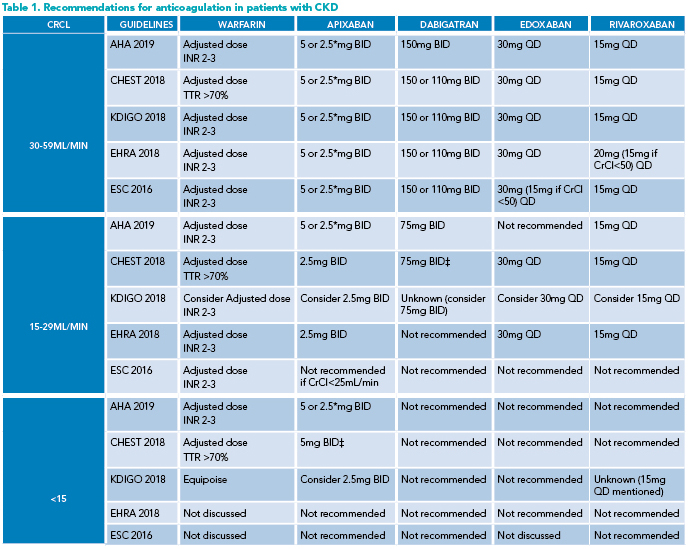
*Use apixaban 2.5 mg BID if any two patient characteristics are present: Cr >1.5 mg/dL (133 mmol/L), >80 years of age, body weight <60 kg. Apixaban is not recommended in patients with severe hepatic impairment. ‡In the United States only. AHA: American Heart Association. BID: twice a day. EHRA: European Heart Rhythm Association. ESC: European Society of Cardiology. INR: International normalized ratio KDIGO: Kidney disease: improving global outcomes. QD: once a day. TTR: time in the international normalized ratio target range.
References
Kumar S et al. Anticoagulation in concomitant chronic kidney disease and atrial fibrillation: JACC review topic of the week. J Am Coll Cardiol. 2019 Oct 29;74(17):2204-2215.
Mavrakanas TA et al. Direct oral anticoagulants in chronic kidney disease: an update. Curr Opin Nephrol Hypertens. 2020 Sep;29(5):489-496.
Weber J et al. The efficacy and safety of direct oral anticoagulants in patients with chronic renal insufficiency: A review of the literature. Eur J Haematol. 2019;102(4):312-318.
Aursulesei V, Costache II. Anticoagulation in chronic kidney disease: from guidelines to clinical practice. Clin Cardiol. 2019;42:774-782.
Siontis KC et al. Outcomes associated with apixaban use in end-stage kidney disease patients with atrial fibrillation in the United States. Circulation. 2018;138:1519-29.
Shin J-I et al. Risks and benefits of direct oral anticoagulants across the spectrum of GFR among incident and prevalent patients with atrial fibrillation. Clin J Am Soc Nephrol 2018;13:1144-1152.
Ando G, Capranzano P. Non-vitamin K antagonist oral anticoagulants in atrial fibrillation patients with chronic kidney disease: a systematic review and network meta-analysis. Int J Cardiol. 2017;231:162-9.

Dr. Viquez-Beita
Dr. Viquez-Beita is an associate professor of medicine at the University of Kentucky College of Medicine in Lexington, Ky.

Dr. Chadha
Dr. Chadha is an associate professor of medicine, assistant dean for competency assessment, and director of the residents as teachers program at the University of Kentucky College of Medicine in Lexington, Ky.