The risk for death goes up for patients with atrial fibrillation (AFib) who are put on direct oral anticoagulants (DOAC) at dosages other than those approved for stroke prevention, whether higher or lower than doses specified in the labeling, suggests a large registry study.
A quarter of more than 10,000 patients in the registry took the drugs at such nonrecommended higher or lower dosages. Overwhelmingly it was the latter, perhaps reflecting caution on the part of some practitioners looking to minimize the risk of bleeding complications.
The risk of major bleeding indeed dropped sharply for those taking DOACs at lower-than-recommended levels, but at the cost of a 25% jump in all-cause mortality over 2 years, report investigators from their analysis of patients in the GARFIELD-AF registry published Sept. 14 in the Journal of the American College of Cardiology.
Risks of major bleeding and of stroke or systemic embolism didn’t climb significantly for patients either under- or overdosed.
In general, “physicians are worried about giving too much anticoagulant, and they tend to favor erring on the low-dose side,” lead author A. John Camm, MD, St. George’s University of London, said in an interview. That’s how it was when an oral anticoagulation meant a vitamin K antagonist (VKA) and underdosing was frequent; and it remains an issue in the DOAC era. “It’s not just a little problem. It’s a very big problem.”
Today, clinicians may prescribe DOACs similar to how they prescribed VKAs, by cautiously choosing a lower dosage for selected patients based on their risk profile, Dr. Camm observed. But in contrast to the VKAs, the DOACs “were studied with different dose-reduction strategies, and their labeling requires them to be prescribed according to different parameters.”
They variously base dosage reductions on age, body weight, renal function, or drug-drug interactions, for example, but some clinicians “tend to think that all of those factors should be applied in every instance, with every drug,” he said.
“So I think there’s some confusion and a lot of caution that physicians use with anticoagulants, and they often forget that the purpose of the anticoagulant is to prevent strokes and adverse outcomes such as mortality,” Dr. Camm said. “But by reducing the dose, they expose their patients to these other major cardiovascular events.”
Numerically, the excess mortality among underdosed patients appeared to be driven by death from heart failure or myocardial infarction. There was little or no contribution from sudden death, fatal strokes, or noncardiovascular death.
The findings “remind clinicians to dose DOACs properly and that there are consequences of dosing errors,” observes Gerald V. Naccarelli, MD, of Penn State University and the Milton S. Hershey Medical Center, Hershey, in an accompanying editorial.
Based on the major clinical trials that established the drugs as mainstream stroke-preventive therapy in AFib, as well as extensive regulatory review, each DOAC’s label-recommended dosing “is a guidance of the truth to achieve the highest efficacy and most safety in our patients,” Dr. Naccarelli wrote. “As clinicians are risk adverse, underdosing might result in lower major bleeding rates, and physicians are blamed for bleeding but not necessarily for allowing embolic strokes to occur. These data raise the issue that underdosing is associated with worse patient outcomes.”
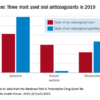
The GARFIELD-AF analysis covered 10,426 adults with nonvalvular AFib in 35 countries who initiated a DOAC from 2013 to 2016. The drugs were prescribed at dosages consistent with recommendations in each respective country’s labeling for stroke prevention in AFib in 72.9% of the cohort. Most full and adjusted dose levels approved by the European Medicines Agency, Food and Drug Administration, and regulators in Japan were the same or similar.
But there were a few exceptions. All dosing criteria across the three regulatory domains were the same for apixaban (Eliquis). But variations included lower dosage options for rivaroxaban (Xarelto) and edoxaban (Savaysa, Lixiana) in Japan, and a uniquely low dabigatran (Pradaxa) dosage option in the United States.
The DOAC used least often was the one most frequently underdosed. More than half of patients prescribed edoxaban were given it at a lower-than-recommended dosage.
The adjusted hazard ratio for all-cause mortality at 2 years for DOAC under- or overdosing, compared with dosing at recommended levels, was 1.24 (95% confidence interval, 1.04-1.48). The difference was driven by underdosing, for which the HR was 1.25 (95% CI, 1.04-1.50). The HR for over-dosing was only 1.19 (95% CI, 0.83-1.71).
Multivariate adjustment accounted for age, sex, and ethnicity; type of AFib; diabetes; hypertensiontransient ischemic attack, or systemic embolism; heart failure
The risk of stroke or systemic embolism didn’t go up or down significantly for either overdosed or underdosed patients. Neither group showed an increased risk for major bleeding; however, the HR for major bleeding in underdosed patients fell to 0.50 (95% CI, 0.28-0.88). Underdosing was more common in some world regions than others. The rate exceeded 30% in all Latin American countries except Argentina, the report stated, and in all Asian countries except Singapore. Japanese patients have long received oral anticoagulation at lower dosages than are used in the West, Dr. Camm observed. When VKAs were the only choice, for example, international normalized ratio targets were consistently a bit lower in Japan than in, for example, North America or Europe. “And when [novel] OACs were developed, again, the Japanese took the view that their patients are more vulnerable to bleeding, and therefore a lower dose would be appropriate. In some instances, lower-dose regimens have been specifically studied in the Japanese,” Dr. Camm said. “Having said that, this concept of bleeding being more problematic in Asian patients has expanded well beyond Japan, and therefore in many Asian communities, lower doses of [novel] OACs are chosen.” Many other factors may contribute to DOAC underdosing, including differences in dosing strategies between primary care practitioners and specialists, or between hospital-based and office-based clinicians, for example. “It might also be argued that a physician who fails to treat a patient adequately in one arena may also be failing to treat the patient well in other aspects of their care,” Dr. Camm proposed. “Therefore you could have increased mortality due to other cardiovascular causes, or even noncardiovascular events, through absence of good quality care. Our study did not address that specifically. But it might be the case, speculatively.” The study was supported by a grant from Bayer to the Thrombosis Research Institute, “which sponsors the GARFIELD-AF registry.” Dr. Camm discloses receiving grants and personal fees from Bayer, Boehringer Ingelheim, Pfizer/Bristol-Myers Squibb, and Daiichi Sankyo. Disclosures for the other authors are in the report. Dr. Naccarelli disclosed consulting and participating in research for Janssen and serving as a consultant for Milestone, Sanofi, Omeicos, and Acesion Pharma. A version of this article originally appeared on Medscape.com.